- Download PDF File
METRICS
- Proceedings of 3rd International Keloid Symposium, Beijing, China, April 19-21, 2019 (887 downloads )
- Post Views: 2,966
- Email Article
Proceedings of 3rd International Keloid Symposium, Beijing, China, April 19-21, 2019
Michael H. Tirgan, MD
Setting the Scene:Basic Understanding of Keloid Disorder
Clinical Presentation And Overview Of Keloid Disorder
Michael H. Tirgan, MD
INTRODUCTION
Keloid Disorder (KD) is an inherited wound healing ailment, frequently seen among Africans /African Americans and Asians. KD has a fascinating and very diverse presentation. In some cases, the disease is limited to one or few small lesions of the skin; either round or linear; in other cases, keloids can appear as large nodules, the conglomerate of nodules, or appear as very large patches or tumors. Such a diverse presentation is most likely tied to a complex and poorly understood genetics. Keloids develop in genetically predisposed individuals as a consequence of injury to the skin that acts as a triggering factor for the formation of the keloid lesions. The triggering factors range from minor inflammatory skin reactions seen with acne, chicken pox, vaccination; or from body piercing, surgical wounds, burns, etc. Although reported in individuals from almost all ethnic backgrounds, the disease is more common among two distinct and genetically distant populations; Africans / African Americans and Asians. Much more research needs to be done to determine the genetic roots of keloid disorder. Lack of progress in keloid disorder is in part due to lack of a lobbying group for this condition. Although quite common, keloid has not captured the interest of research community. This needs to change.
The Establishment Of Keloid Comprehensive Diagnosis And Treatment System
Xiaojun Wang, MD
Keloid is one kind of benign skin tumor with invasive growth like malignant tumor. Keloid could happen in any part of the body, companied with unbearable itch and pain which seriously affect patients’ life quality and mental health. In addition, infection and ulcer often occur on keloid, and turned into scar cancer with poor prognosis and high death rate. The early stage appearance of keloid is not particular which caused difficulties in keloid diagnosis. High recurrence after simple surgical excision is also another characteristics of keloid. In this case, keloid had become one of the most difficult world-wide problem in plastic surgery field. Based on those facts above, our team had accomplished a series of preclinical researches and clinical practices.
In preclinical researches of gene and cell aspects, our team found that keloid tissue underwent hypoxia microenvironment with high expression of HIF-1α which induced the EMT phenomenon of keloidderived keratinocytes, and firstly established EMT cell model on keratinocytes, and explored the LncRNA target factor between keloid and normal skin tissue. Furthermore, HIF-1α has also been studied. HIF-1α has been proved the key factor that promoted EMT phenomenon. Increasing radiotherapy sensitivity of keloid fibroblasts had also been found when blocking HIF-1α. 2ME2 has inhibitory effect towards the expression of HIF-1α, cell activity and radiotherapy sensitivity. Our results demonstrated hypoxia environment caused the EMT phenomenon and lead to invasive growth. LSCI was firstly used to evaluate the inner characteristics of keloid blood perfusion. The blood perfusion is higher in keloid tissue. There are also changes in normal skin tissue around keloid, and different scar types also appear different blood perfusion level. This project objectively established new classification and clinical diagnosis standards of keloid.
This project also focus on the clinical translation. According to the inner blood perfusion changes, this project established objective classification of keloid. Doctors could use different clinical approaches and adjunctive therapies according to this classification. A keloid precut, pre-radiotherapy has also been used for large keloid, which assured the effective dose of radiotherapy and decreased recurrence. Hyperbaric oxygen therapy has also been firstly applied in plastic field towards the hypoxia environment of keloid, which effectively ameliorated local inflammation and EMT phenomenon.
After fifteen years of analyzing pre-clinical researches and summarizing clinical practical experiences, our team has established keloid comprehensive diagnosis and treatment system which modified keloid clinical diagnosis standard, enriched treating approaches and reduced keloid recurrence. The accomplishment of this project stands leading level in China or even the world and approved by many industry experts, which also been promoted through experts public welfare tour of Chinese medical association. The promotion with satisfying social benefits, including nearly 10,000 people, were held in more than 20 areas like Changchun, Wuhan, Xinjiang, Qinghai, Ningxia and Anhui, which improved the whole level of keloid diagnosis and treatment in China.
Keloid Link To Breast Cancer Outcomes; Suggests Ethnic Variation In Immune Response & Tumor Behavior
Lamont R Jones MD, MBA1, Edward M Walton BS2, Brittany D Jenkins PhDc3, Vanessa P Chu BA2, Haythem Y Ali MD4, Christine M Nesland-Dudas PhD3, Eleanor M Walker PhD5, Melissa B Davis PhD3
The project was performed at Henry Ford Health System in Detroit, Michigan, USA.
This project was presented as an oral presentation at the 2019 Triological Society Combined Sections Meeting in Coronado, CA, January 24-26, 2019. Funding and Conflicts of Interest: The authors have no financial disclosures or conflicts of interest to report. Send correspondence to Lamont R. Jones, MD, MBA, Department of Otolaryngology–Head and Neck Surgery, Henry Ford Hospital, 2799 West Grand Blvd., Detroit, MI 48202; Telephone: (313) 916-5722; E-mail: ljones5@hfhs.org.
Objective: It is known that keloids and aggressive breast cancer (BC) disproportionately affect African Americans (AA). The former is a benign fibroproliferative tumor characterized by malignantlike features but does not cross the threshold to malignancy. The latter is often associated with poor survival in AAs due to the predominance of triplenegative and inflammatory subtypes. These disparities may be explained in part by ethnic variations in tumor microenvironment, which involve tumor inflammatory responses. We hypothesized that AA women with a history of keloids would reflect a population of BC patients with aggressive tumors and poor outcomes.
Methods: Medical record review of 13,033 patients with scar codes diagnosed between 2005-2015 was conducted. Of these, 283 had a concurrent BC diagnosis where 152 were screened keloid-negative and 103 were keloid-positive. Using this 283-patient cohort, we conducted multivariate screening to identify epidemiological associations between BC related clinical factors and keloid status. Analysis was done using SAS-derived software, JMP v13.0
Results: We found a race-specific age association with AA patients displaying significantly younger ages at diagnosis in keloid-positive patients (mean 52y) compared to keloid-negative patients (mean 58y) (P=.021), while European Americans patients had no difference in age (mean, 59y vs. 55y) (P=.333). We also observed a significant difference in tumor staging (P=.047).
Conclusion: Keloid status of an individual may be indicative of a risk to be diagnosed with early-onset, late staged BC. In addition, it was a distinguishing factor among AA women, which may point to a pathological/molecular pathway that predicates their unique cancer risk.
Psycho-Social Impact Of Patients With Keloids
Kamalendu Malaker 1,2,3,4,5, Nandan Shanbagh1, Mustafa Zaidi2, Rida Franka2, Twafie Alyaffi3
INTRODUCTION
Four (4) patients sought treatment for their keloids for “non-clinical” reasons, and to improve their lifestyles. The patients include a 28 year male who is a fourth year medical student, a 28 year old woman who is the daughter of a wealthy businessman, a 25 year old woman who is the daughter of a high ranking military general, and a 43 year old female nurse. All of them requested treatment of their keloids for “psycho-social” reasons.
MATERIALS AND METHODS
The above four patients highlighted the urgency of psycho-social evaluations and management of patients with keloids, even though they had no apparent physical symptoms. As a result, a psycho-social questionnaire has been appended to the standard history and physical examination documentation.
RESULTS
Nineteen patients were evaluated, including 14 females (18 to 49 years old), and five male (26 to 38 years old). The findings were that all patients, irrespective of sex and age, admitted a psychological affliction and perception of social deprivation and isolation. Men felt more discrimination at work place. Nine patients, who could be tracked one year after treatment, all reported to have a normal self-esteem and social integration.
CONCLUSION
Psycho-social affliction is a real clinical issue in a high number patients with keloids. These are relieved after successful treatment leading to happy and productive lifestyles. Hence, patients with untreatable keloids deserve early attention to address and mitigate their silent suffering from psycho-social ailment to restore normal life style and be productive and happy members of the society.
In Vivo and in Vitro Models for Keloid Research
The Use Of Induced Pluripotent Stem Cells (iPSCs) In Keloid Research
Shyam K. Sah PhD, Jitendra Kanaujia PhD,
Samuel Ademola MD, Solomon Fadiora MD,
Peter B. Olaitan MD, Odunayo M. Oluwatosin
MD, Ernst J Reichenberger PhD
Keloid formation is unique to humans and while keloid growth has many parallels with other fibrotic disorders, the initiating factors that drive keloid formation are still unknown. Models for keloid research range from studies on isolated fibroblasts or keratinocytes from patients to transplanting keloid scars into immunodeficient mice. The model spectrum also includes gene over-expression or knock-down approaches in cell lines or wound healing studies in knock-out mice. Recently it became possible to generate induced pluripotent stem cells (iPSCs) from somatic cells of patient. iPSCs can be differentiated into various cell types that have the genetic background and the characteristics of cells from the donor. Similarly, mutations can be introduced into iPSCs by CRISPR/ Cas techniques to study disease-causing genetic variants when tissues from patients are not available.
Instead of studying general fibrosis pathways of keloid patients with unknown genetic background, we are interested in the genetic basis of inheritable keloids. We previously identified genetic variants in affected members of Nigerian keloid families. Because keloid tissue from those patients is not available to study the effect of variants on tissue fibrosis we needed to generate model systems. We chose to introduce keloid variants into well-characterized iPSCs and differentiate those into fibroblasts and keratinocytes. Cellular properties of mutant lines can then be compared to properties of the original iPSC line. Except for the variant, both cell lines are genetically virtually identical. This strategy eliminates genetic heterogeneity, which often hampers comparison between primary cell lines.
We use iPSC-derived cells for cellular assays or for organotypic 3D skin equivalents. We are, for example, interested in a non-synonymous variant in the acid ceramidase ASAH1 (N-acylsphingosine amidohydrolase) that appears to reduce its ceramidase activity. ASAH1 is expressed mostly in the epidermis and is one of the enzymes that controls the ratio of ceramide and sphingosine. iPSC-derived fibroblasts show increased proliferation rate, collagen synthesis and susceptibility to TGF-β stimulation. In summary, iPSCs may be a good model system to study keloids in a controlled cellular environment.
Keloid-Associated Lymphoid Tissues In Keloid Lesions Express Vitamin D Receptor
Swee T. Tan1, 2, Ethan Kilmister1, Kim H Lim1, Tinte Itinteang1, Bede van Schaijik1, Helen D Brasch1, Paul F Davis1
Objectives Vitamin D receptor (VDR) may play a role in keloid disorder. This study investigated the expression of VDR by the embryonic stem cell (ESC)- like population within keloid-associated lymphoid tissues (KALTs) which expresses components of the renin-angiotensin system (RAS).
Methods 11 formalin-fixed paraffin-embedded sections of keloid lesions (KLs) underwent 3,3-diminobenzidine (DAB) immunohistochemical (IHC) staining for VDR. Immunofluorescence (IF) dual IHC staining of CD34/VDR and OCT4/ VDR was performed on two representative KLs. Transcriptional activation of VDR was investigated in four representative snap-frozen KLs using real-time
polymerase chain reaction (RT-qPCR).
Results DAB IHC staining demonstrated the presence of VDR on the KALTs within the keloid tissue samples. RT-qPCR confirmed transcriptional activation of VDR. IF IHC staining demonstrated expression of VDR on the CD34+ and the OCT4+ endothelium of the microvessels, and the OCT4+ perivascular cells, within the KALTs.
Conclusions This study demonstrated the expression of VDR by the ESC-like population within the KALTs in KLs. Further work is needed to elucidate the precise interaction between VDR and the RAS in regulating the primitive population within KALTs.
Contact Information: Dr Swee T Tan ONZM MBBS PhD
FRACS, Gillies McIndoe Research Institute, PO Box 7184,
Newtown 6242, Wellington, New Zealand. Ph: +64 4
2820366 Em: swee.tan@gmri.org.nz
Ethics Committee Approval: This study was approved by the Central Health and Disability Ethics Committee (Ref. 13/ NTB/155) with written informed consent from all subjects in accordance with the Declaration of Helsinki.
Original Research: This is an original research Funding: This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors. Ethan Kilmister was supported by a summer scholarship from the Deane Endowment Trust.
Disclosure Declaration: Drs Tinte Itinteang, Paul Davis and Swee Tan are inventors of a PCT application Treatment of Fibrotic Conditions (PCT/NZ2016/050187). The authors are otherwise not aware of any commercial associations or financial relationships that might pose or create a conflict of interest with information presented in any submitted manuscript.
A Comparison Of Apoptosis Levels In Keloid Tissue, Physiological Scars And Normal Skin
Hao Liu, MD
Apoptosis is a process of programmed cell death that occurs in multicellular organisms. The mitochondrial pathway plays a paramount role in apoptosis. In this study, the expression levels of key factors in the mitochondrial pathway and the cell proliferation factor (PCNA) were measured to evaluate the level of apoptosis and proliferation in keloid scars, physiological scars and normal skin tissue. Thirty samples were taken from 30 patients: 10 keloid patients, 10 physiological scar patients and 10 patients without obvious scarring. Hematoxylin and eosin staining and Masson staining were used to observe the differences in histology and fiber tissue content. Mitochondrial pathway factors (caspase-3, caspase-8, caspase-9, Bcl- 2, Bax, cytochromec) and PCNA expression levels were detected by immunohistochemistry and were analyzed as the percentage of positively stained cells in the epidermis and dermis. Relative protein expression levels were measured by western blotting. Compared with physiological scars and normal skin tissue, keloid tissue had an increase in fiber number and decrease in cell content. In our immunohistochemical and western blot analyses, all tissue types showed similar expression levels of the mitochondrial pathway factors. However, the percentage of PCNA-positive cells and the relative protein expression level of PCNA were significantly higher in keloid tissue. Keloid has a similar apoptosis level as physiological scars and normal skin but has a higher expression of PCNA, indicating that keloid scars have high levels of proliferation and normal apoptosis.
Aligned Topography Mediated Cell Elongation Reverses Pathological Phenotype Of Vitro Cultured Keloid Fibroblasts
Jia Huang MD
Abstract:
Topography modifying cell behavior remains less explored in diseased cells. This study investigated the reversing effect on the pathological phenotype of keloid fibroblasts via culturing cells on a parallel microgrooved surface. The results showed that this particular topography with 3 μm groove depth and 10 μm width could significantly elongate and align the cultured cells with reduced cell (nucleus) area and increased cell(nucleus) body aspect ratio and cell (nucleus) body major axis (p<0.05). Importantly, the elongated cells gradually lost their fibrotic phenotype with inhibited cell proliferation and cell cycle arrest in S-phase (p<0.05), reduced expression of fibrotic markers such as collagen, fibronectin, CTGF, α-SMA, TGF-β1 (p<0.05) and increased MMPs/TIMP-1 ratio (p<0.05) along with attenuated Smad and Erk phosphorylation level. All these indicate that this parallel topography is power enough to modify keloid cell phenotype, a benign skin tumor with excessive cell proliferation and matrix production.
Fibroblast- Macrophage Interaction As A Lever For The Resolution Of Keloid Fibrosis
Rolin G.1,2,*, Thomas Cherrier2, Melissa Maraux2, Etienne Daguindau2, Jamal Boumalid2, Sylvain Perruche2
* Contact information
Dr. Gwenaël ROLIN, PhD, Hospital Research Engineer
INSERM CIC-1431, University Hospital of Besançon,
Clinical Investigation Center 2 place St Jacques –
25000 Besançon
grolin@chu-besancon.fr
Office: +33 (0)3 81 21 91 64 / Mobile: +33(0)6 84 25 77 92
Macrophage is one of the key cells in the process of tissue fibrosis (TF). Tts plasticity makes itself an ideal target for TF prevention and resolution. After an injury, human body sets up an inflammatory response to protect itself from viruses and bacteria. Then, inflammation naturally stops thanks to the initiation of neutrophils apoptosis. In response, monocytes are attracted into the wound sites, migrate inside the tissue, differentiate into macrophages and clean the wound. During this phase, macrophages eliminate apoptotic cells and then release various factors allowing two major simultaneous actions: 1) put an end to inflammation and 2) initiate tissue repair by recruiting fibroblasts and epithelial cells. Both of these two major actions constitute the process of inflammation resolution. However, this process has been described to be altered in many chronic inflammatory diseases (systemic scleroderma in skin, sclerosis in central nervous system, Crohn’s disease in intestine or rheumatoid arthritis in joints). In the fibrosis context, chronic inflammation releases factors (VEGF, PDGF), enzymes (caspase) and pro-fibrotic cytokines (IL-13, IL-21, TGF-β1) that promote overproduction of connective tissue. On the contrary, when tissue repair is well modulated, following a quickly-resolved inflammatory response, the normal architecture of the tissue is restored. If tissue repair is dysregulated pathological fibrosis appears.
Macrophages are a heterogeneous population of immune. Macrophages exhibit a great plasticity and can adopt various phenotypes with antagonistic functions.
For example, they can promote inflammation by secreting TNF-α, IL1-β, IL-6 or nitric oxide but also stop inflammation by secreting pro-resolving factors (TGF-β, IL-10, Resolvin …). This plasticity has been shown to be dependent on the microenvironment in which they are located. Thus, for example TNF-α and IFN-γ will induce a pro-inflammatory phenotype called “M1-like” and IL-4, IL-10 or IL-13 will induce an antiinflammatory phenotype called “M2-like”. Interestingly a macrophage phenotype can be reversed with appropriate signals. To our knowledge, few data are available about the types of macrophages present in fibrotic tissue in humans. The dual action of the macrophage has been demonstrated mainly in murine models. In the context of keloids, the number of cells of Langerhans (CD1α +), T cells (CD3 +), macrophage (CD38 +) and B cells (CD20 +) is increased in the keloid tissue compared to healthy skin. More recently, it has been confirmed that the keloid tissue contains more M2 (CD14 +) and T (CD3 +) macrophage than healthy skin, demonstrating the potential involvement of macrophages sub-family in keloid pathology. In addition, the transcription and protein expression of iNOS, IL-12, IL-10 and TGF-β was described to be enhanced in keloids macrophages. Unfortunately, there are few data in the literature about the role and function of macrophages in the keloid pathogenesis as well as its cross-talk with fibroblasts. In light of the available knowledge and previously published data on the role of the macrophage in the development of tissue fibrosis, we hypothesize that plasticity and reprogramming of macrophages can be a powerful lever for the prevention and resolution of keloid fibrosis.
Shaker, S. A., N. N. Ayuob and N. H. Hajrah (2011). “Cell talk: a phenomenon observed in the keloid scar by immunohistochemical study.” Appl Immunohistochem Mol Morphol 19(2): 153-159.
Slemp, A. E. and R. E. Kirschner (2006). “Keloids and scars: a review of keloids and scars, their pathogenesis, risk factors, and management.” Curr Opin Pediatr 18(4): 396-402.
Jin, Q., L. Gui, F. Niu, B. Yu, N. Lauda, J. Liu, X. Mao and Y. Chen (2018). “Macrophages in keloid are potent at promoting the differentiation and function of regulatory T cells.” Exp Cell Res 362(2): 472-476.
Wynn, T. A. and K. M. Vannella (2016). “Macrophages in Tissue Repair, Regeneration, and Fibrosis.” Immunity 44(3): 450-462.
Overall Strategy for Management of Keloid Patients
Decision On The Proper Strategy Of Keloid Therapy: The Key For Successful Treatment Of This Disease
Wei Liu, MD
Keloid is a disease difficult to cure due to its high recurrence post various therapies and resistance to different therapeutics. The most likely reason for this phenomenon is the lack of proper understanding of this disease comprehensively. Despite substantial efforts of basic researches have been made to understand the molecular mechanism using cell biology approaches, relatively less progress is made in clinical therapy using basic research findings. The shortcomings of many unproper strategies include single-molecule based therapy, monotherapy approach, local therapy without systemic consideration, etc. To design a proper keloid therapeutic strategy, global reasoning sense should be employed to integrate as many as possible elements into an integrative therapeutic approach. Essentially, keloid is a disease unique to human being, which means that environmental factors play essential role and keloid won’t occur when cells are deprived from these environmental factors. Therefore, environmental therapy must be included in keloid therapeutic strategy. Secondary, integrative therapy should be employed to cover anti-inflammation, anticell proliferation, anti-matrix production, anti-cell migration/invasion. Third, multi-therapy modality should be employed to enhance therapeutic efficacy and reduce side-effects. Fourth, sustainable approach should also be used simply because relatively long therapeutic time is needed to completely cure keloid without recurrence. This presentation would like to propose these concepts for properly design keloid therapeutic strategies.
The treatment of keloid and hypertrophic scars in a scar clinic, a retrospective study
F.B. Niessen, MD, PhD1, T. Fakkel, MD1, F. Heijsters, MD1
BACKGROUND
More than 100 million people in the developing countries suffer from hypertrophic scars and keloids. Treatment is very challenging because of the high recurrence rate and the high rate of complications. Although many treatment modalities are available, none of them is satisfying and consensus about effectivity is lacking.
In this retrospective study we looked at the effectiveness of different treatment protocols in the ‘ScarClinic’ AUMC in the last year.
METHODS
This retrospective study is performed after data acquisition of patients treated between May 2017 till September 2018 in the ‘ScarClinic’ AUMC. Only patients with hypertrophic scars and/or keloids were included. Both patient characteristics as well as treatment characteristics were studied. Patients were divided in 7 treatment protocols and got mono- or combination therapy. Outcome regarding recurrence and complications were studied. Pearson chi-squared test and ANOVA were used.
RESULTS
309 patients were treated, of which 225 keloid and 53 hypertrophic scars. 62.8% of the study population was female with a mean age of 27 years. 62.1% was treated in another hospital. 90/309 patients got monotherapy (Kenacort, cryotherapy, brachytherapy, excision, silicone application, tattoo, Cetirizine, Doxycyclin, Diet) and 211 /309 a combination of at least two therapies. 8 /309 no therapy.
57/301 patients developed a recurrence, of which 23 (25.6%) following monotherapy (13 after Kenacort, 5 after brachytherapy) and 34 (16.1%) following polytherapy. (Kenacort and cryotherapy). 10/57 patients with a recurrence could be successfully treated with Kenacort. The difference was almost significant. (p = 0.056)
DISCUSSION
In this retrospective large case series, it can be concluded that polytherapy has an almost significant lower recurrence rate in the treatment of hypertrophic scars and keloids compared to monotherapy. Due to the retrospective nature of this study, both groups were not comparable. These results have to be taken with care, but our advise would be to treat excessive scar formation multimodal.
The Strategy Of Keloid Therapy- The Experience Of Shanghai 9Th Hospital
Xiaoli Wu, MD
Keloid is a complex and frustrating disease, and its occurrence and development are affected by multiple factors. The treatment of keloids includes drug injection, surgery, radiotherapy, laser, etc. Treatment with either method alone can lead to the recurrence of keloids. The choice of treatment plan is influenced by various factors such as the clinical classification of keloids and the patient’s own conditions. We have achieved good results in combination with various methods in clinical practice.
KRF Clinical Practice Guideline – Treatment Strategy
Michael H. Tirgan, MD
INTRODUCTION
It has long been known that successful treatment of a disease is possible only when we understand the underlying pathophysiology. Certain de-novo skin pathologies, for instance basal cell carcinoma, can be successfully treated with surgery. However, postoperative recurrence is observed in almost 100% of patients undergoing keloid removal surgery, hence adjuvant ILT or radiation therapy are incorporated to reduce the risk of recurrence. The core question to ask is, “Why is there such a high rate of recurrences after keloid removal surgery?” The answer is that keloid removal surgery starts with, and imposes, a totally new wound and a new injury to the skin, thereby triggering the same keloidal wound healing response that produced the original keloid. Perhaps, this is the only medical condition that is triggered, and even made worse, by surgical treatment.
Focus on keloid patient and not on the keloid lesion
Exposure to radiation therapy and/or frequent injections of high-dose steroids are known to result in long-term, significant, adverse effects. The practice of radiating benign skin conditions was abandoned several decades ago because of the increased incidence of fatal cancers.
Considering the above risks, our strategy should focus on treating the keloid patient as opposed to removing a keloid lesion. We need to focus our attention on reducing the risk of harm to the patients by carefully crafting treatment plans that place the focus on the patient and not on excising a keloid lesion and doing everything we can to prevent recurrence at the surgery site.
Data-driven treatment pathways
The biggest handicap to treating keloid patients is the lack of data-driven treatment pathways. Despite the abundance of patients with all types of keloids, there is a paucity of properly designed and well conducted clinical trials that can form the foundation for proper clinical management of patients with different types of keloids.
Setting treatment goals
Treatment strategy starts with establishing the treatment goals, which often varies from patient to patient. A young person with a small facial keloid would most likely desire to see its total disappearance; yet on the other hand, an elderly patient with a poststernotomy keloid may only desire symptom control. Once the treatment goals are established, patients should be educated about details of each treatment modality that and all potential side effects.
Treatment tools:
Current treatment Guidance and KRF recommendations are based on the following methods of treatment.
- Intra-Lesional Triamcinolone (ILT)
- Intra-Lesional Chemotherapy (ILC)
- Contact Cryotherapy
- Pressure devices
At the current time, KRF advises against surgery, radiation therapy, and laser treatment. KRF’s recommendations are for the most part based on reducing the risk for the iatrogenic worsening of the keloids.
Aggressive treatment of early stage disease
All keloid lesions start as a small papule or a minor liner lesion. The correct approach to such early-stage keloid lesions is to treat them very aggressively with the goal of inducing a complete remission. It is only with this approach that we can have a significant impact on the natural history of this disorder. Quite often a keloid papule does not receive proper treatment and as a result, it grows to becomes a nodule or a small tumor. Often, at that point, a decision is made to remove the lesion surgically. Preventing keloid papules to go down this treatment approach is the cornerstone of successful treatment of keloid patients because allowing a keloid papule to grow and to form a nodule, and removing that nodule surgically, is a path that only leads to the formation of life changing keloids.
Abstract Presentations
Can Keloid Lesions Be Ascribed? Examining The Relationship Between Keloid Disorder, Perceived Psychosocial Distress, And Plasma Neuropeptide Y
Alison T. Tran1, M.A., Ed.M, Lynn Copes, PhD
Frank H. Netter MD
BACKGROUND
The relationship between the mind and skin has long been hypothesized to exist as the brain and skin share embryologic ectodermal origin and are affected by similar neuro-hormonal factors [1]. Understandably, there is psychiatric co-morbidity in approximately 30- 40% of dermatologic patients, which is slightly higher than that of neurologic, oncologic and cardiac patients combined [1]. Chronic experience of stress may lead to adverse health outcomes in the form of “stressrelated disease,” a term first coined by Hans Seyle [2].
Neuropeptide Y (NPY) is often regarded as the stressmediated “resilience peptide.” As a pleiotropic factor, NPY exerts diverse effects across many systems. NPY has distinct actions centrally and peripherally. In the central nervous system, it inhibits sympathetic activity [3], is anxiolytic and antiepileptic [4]. It enhances stress coping abilities [5] and resilience to stress as it is abundantly expressed in brain regions known for stress and emotional regulation [6]. Peripherally, it is pro-stress and vasoconstrictive.
NPY secreted from nerve fibers in skin can modulate functions of cutaneous and/or immune cells [5]. Exogenous and endogenous stress may induce the release of NPY, which may lead to enhanced immune response via lymphocyte proliferation; in turn, lymphocytes and macrophages produce NPY once activated [cite]. A role for NPY in the pathogenesis of vitiligo has been proposed after elevated NPY levels were found in the depigmented skin [6, 7] and plasma of individuals with vitiligo [8], indicating 1 School of Medicine at Quinnipiac University 370 Bassett Rd, North Haven, CT 06473 Alison.tran@quinnipiac.edu a possible relationship between NPY, lymphocytic proliferation and subsequent melanocytic destruction [7]. Of particular importance to the pathogenesis of keloid disorder is the M2 macrophage, which specifically regulates wound repair. In addition, NPYdependent angiogenesis plays a role in wound healing, vascularization in ischemia, aging, and induces basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF) expression [9].
Race Beyond Genetics: Effects of discrimination and stress on the body
Manifestation of illness can extend beyond race and be attributed to epigenetics. There is an extensive body of research on the effects of psychosocial stress/ discrimination and hormones on the body. Selfreported discrimination at the individual level has been linked to a wide range of health issues such as elevated blood pressure, breast cancer, preterm delivery/low birth weight and depression [10]. Gravlee (2009) argues that racial inequalities “become embodied” in the biological well-being of racialized groups/ individuals as the sociocultural reality racism has biological consequences for racially defined groups.
Keloid lesions are generally more common in darker pigmented skin [9], specifically, in African, Latin American [11] and Asian American [12] individuals. About 4-16% of darker pigmented individuals report decreased physical and/or mental health due to pain and disfigurement accompanying keloids [11]. The purpose of this study is to investigate the relationship between keloid disorder, psychosocial distress associated with ascribed status (social status assigned at birth) and NPY, specifically its role in stress mediation, angiogenesis and wound repair.
Method: A total of 37 (15 men, 22 women) Black, Hispanic and Asian volunteers with and without keloids participated in this current study. The experimental group consisted of keloid formers (8 males, 12 females) and the control group consisted of non-keloid formers (7 males, 10 females). Participants were asked to provide information about their current health, income and experience with trauma/ discrimination as well as complete a 22-item Psychological General Well-Being Index (PGWBI) and a 10-item Dermatology Life Quality Index (DLQI). Following this, participants had 2 ml of blood drawn via venipuncture before and after watching a stress-inducing video. NPY levels pre/post video were analyzed using commercially available ELISA kits.
Results: Preliminary results show a potential interaction between gender, race and keloid status, where Black men with keloid disorder showed a more exaggerated response (increased NPY levels) to acute stress (stereotype threat video) compared to Black women with keloid disorder. Moreover, there was a positive correlation between quality of life/stress and keloid status such that subjects with keloids have a higher Dermatology Life Quality Index (DLQI) than subjects without keloids (means of 4.40 vs. 2.65, p=. 040). Further analysis indicated a near significant difference between all four groups (male/no keloid, male/keloid, female/no keloid, female/keloid) and self-reported overall health and Psychological General Well-Being Index (PGWBI).
Conclusion: To our knowledge, no research has been done on the possible relationship between NPY on keloid disorder. Future research should use stricter inclusion criteria in order to control for confounds in order to determine true significance of preliminary results. Additionally, this project aims to raise awareness on the impact of psychosocial conditions on symptomology as well as highlight the possible benefits of incorporating psychotherapeutic tactics and coordinating psychological services within dermatological care.
The Impact Of Matrix Stiffness On Fibroblast Phenotype And Keloid
Zhenjun Deng1, Manon Subilia2, Yu Suk Choi3, Nicole Hortin1, Andrew Stevenson1, Fiona Wood1,4, Cecilia Prele5,6 Mark Fear1
Extracellular matrix stiffness is known as an important micro-environmental cue that regulates cell behaviour and function. Yes-associated protein (YAP) is a key mechanoactivated coordinator of fibroblast activation and matrix deposition and is translocated to the nucleus upon activation by increased stiffness. However, most in vitro research into keloid disease uses cells cultured on stiff petri dishes, which does not effectively mimic the in vivo physicomechanical properties of skin tissue. Here, we have studied the impact of matrix stiffness on fibroblast phenotype by culturing the cells on a stiff coverslip (>109 Pa), 2 kPa polyacrylamide (PA) hydrogel (normal dermisequivalent stiffness), 20 kPa PA hydrogel (keloidequivalent stiffness), and 40 kPa PA hydrogel (extreme pathological-equivalent stiffness). In this study, the expression of α-Smooth muscle actin (α-SMA) was increased with increasing matrix stiffness in both normal fibroblasts and keloid fibroblasts. Moreover, keloid fibroblasts expressed higher α-SMA than normal fibroblasts in all conditions. In normal fibroblasts, matrices of pathologic stiffness induced YAP nuclear translocation as did stimulation with TGF-β. However, in contrast, keloid fibroblasts do not respond to increased matrix stiffness as would be expected. Keloid fibroblasts exhibit hyperresponsiveness to both physiological-equivalent stiffness and pathologicalequivalent stiffness, suggesting that keloid fibroblasts have established an activated state of YAP that is independent of mechanical cues. There is no increase in nuclear YAP in response to increasing stiffness nor to treatment with TGF-β, suggesting the keloid fibroblasts are autoregulated to produce higher levels of collagen irrespective of the physical properties of the matrix.
Taken together, this data shows that normal skin fibroblasts respond to the physical properties of the matrix in vitro. However, keloid fibroblasts appear to have elevated activation of mechanotransduction pathways irrespective of the environment. This change may significantly contribute to the pathogenesis of keloid and has implications for potential treatments to ameliorate keloid disease.
- Author name: Zhenjun Deng
Academic degree: Second year PhD candidature,
Master of Medicine
Email address: 22371151@student.uwa.edu.au - Author name: Manon Subilia
Academic degree: MSc
Email address: manon.subilia@epfl.ch - Author name: Yu Suk Choi
Academic degree: PhD
Email address: yusuk.choi@uwa.edu.au - Author name: Nicole Hortin
Academic degree: BSc
Email address: nicole.hortin@uwa.edu.au - Author name: Andrew Stevenson
Academic degree: PhD
Email address: andrew@fionawoodfoundation.com - Author name: Fiona Wood
Academic degree: FRACS
Email address: Fiona.Wood@health.wa.gov.au - Author name: Cecilia Prele
Academic degree: PhD BSc (Hons)
Email address: cecilia.prele@uwa.edu.au - Author name: Mark Fear
Academic degree: PhD
Email address: mark@fionawoodfoundation.com
Funding: NHMRC, Fiona Wood Foundation
Ethics: HREC
Topical Lysyl Oxidase Inhibitors To Treat Keloid Lesions
Nutan Chaudhari1, Zhenjun Deng1, Nicole Hortin1, Andrew Stevenson1, Emily O’Ryen1, Killugudi Iyer2, Fiona Wood1,3, Wolfgang Jarolimek4, and Mark Fear1
Keloid is a progressive fibrotic disease characterised by ongoing deposition of extracellular matrix and growth of tissue after injury. Collagen production is regulated by both intra and extracellular mechanisms. After collagen is secreted into the extracellular space it is then gets stabilised by formation of crosslinks. Formation of these crosslinks is regulated by a family of enzymes, the lysyl oxidases (LOX). We have developed a pan- LOX inhibitor that effectively reduces crosslinking of collagen both in vitro and in vivo. Here, we describe the effects of a topical LOX inhibitor on keloid cells and its potential for translation into the clinic
Lysyl oxidase levels are elevated in scar and keloid fibroblasts. Collagen production is significantly higher in keloid fibroblasts compared to skin fibroblasts in monoculture. In addition, increased amounts of collagen crosslinks are observed in collagen produced by keloid fibroblasts compared to normal scar fibroblasts. Using the inhibitor of LOX activity (LOXi) demonstrated that collagen cross-linking was reduced in response to treatment. Interestingly, treatment of keloid fibroblasts with LOXi also reduced collagen production when measured using qPCR and a soluble protein assay. This suggests that disrupting the Collagen matrix generates a feedback loop that subsequently reduces collagen production. Finally, topical application of the LOXi to ex-vivo keloid tissue effectively reduced target enzyme activity. Together this data suggests that topical treatment of keloid tissue using a LOXi can reduce collagen stability and subsequent collagen production and may thereby ameliorate keloid progression or recurrence after surgery. Further in vivo studies will be required to confirm these findings and to progress towards a clinical trial.
Funding source: This research is funded by Fiona Wood foundation.
Author details:
- Nutan Chaudhari
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: nutan.chaudhari@research.uwa.edu.au
Qualifications: Third year PhD student - Zhenjun Deng
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: zhenjun.deng@research.uwa.edu.au
Qualifications: Second year PhD student - Nicole Hortin
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: Nicole.hortin@.uwa.edu.au
Qualifications: B.Sc. (Hons) - Andrew Stevenson
Institution: Burn Injury Research Unit, The University of
Western Australia WA, 6009
Email address: andrew.stevenson@.uwa.edu.au
Qualifications: B.Sc. (Hons), PhD - Emily O’Halloran
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: ohalloranemily@gmail.com
Qualifications: M.B.B.S. - Killugudi S. Iyer
Institution: School of Chemistry and Biochemistry, The
University of Western Australia, WA, 6009
Email address: swaminatha.iyer@uwa.edu.au
Qualifications: B.Sc. (Hons), PhD - Fiona Wood
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: fiona.wood@uwa.edu.au
Qualifications: FRCS - Wolfgang Jarolimek
Institution: Burn Injury Research Unit, The University of
Western Australia WA, 6009
Email address: mark.fear@uwa.edu.au
Qualifications: B.Sc. (Hons), PhD - Mark Fear :
Institution: Burn Injury Research Unit, The University of
Western Australia, WA, 6009
Email address: mark.fear@uwa.edu.au
Qualifications: B.Sc. (Hons), PhD
Understanding Activin And Follistatin Pathway In Keloids For Developing A Novel Treatment
Seungmin Ham1,4, Craig Harrison2, David de Kretser3,4, Euan M. Wallace1, Graeme Southwick1,3,5, and Peter Temple-Smith1
Departments of 1Obstetrics and Gynaecology, 2Physiology, 3Anatomy and Developmental Biology, Monash University, Melbourne, Victoria, 3168; 4Hudson Institute of Medical Research, Melbourne, Victoria, 3168; 5Melbourne Institute of Plastic Surgery, Malvern, Victoria, Australia, 3144.
BACKGROUND
Keloids are benign disfiguring tumours caused by abnormal wound healing that is ostensibly driven by increased local expression of cytokines and growth factors, including activin A. This study compared the effects of activins on the function of normal (control) and keloid-derived dermal fibroblasts and investigated the use of follistatin as a novel treatment for keloids.
METHODS
Normal and keloid tissue samples from 11 patients were used to develop primary fibroblast cultures, which were compared in terms of their histology and relevant gene (qRT-PCR and RNAseq) and protein (ELISA) expression.
RESULTS AND DISCUSSION
Activin A gene (INHBA) expression was significantly upregulated in keloid fibroblasts leading to increased activin A protein in cell lysates and culture medium. Connective tissue growth factor (CTGF), a fibrosisrelated gene, was also significantly upregulated in keloid fibroblasts. Activator protein 1 (AP1) inhibitor (SR11302) treatment significantly decreased INHBA and CTGF expression in keloid fibroblasts by diminishing autocrine actions of activin. A single treatment of follistatin over five days significantly downregulated INHBA expression in keloid fibroblasts confirming the autocrine actions of activin A. Follistatin, by inhibiting the actions of activin, significantly inhibited various matrix-related genes in keloid fibroblasts compared to controls.
CONCLUSION
Keloids are linked to local production of activin A stimulated by transcriptional factor AP1. Follistatin, by binding activin A, suppresses CTGF expression suggesting a novel therapeutic role in managing keloids and other fibrotic diseases.
CUDC-907 Reverses Pathological Phenotype Of Keloid Fibroblasts In Vitro And In Vivo Via Dual Inhibition Of PI3K/Akt/mTOR Signaling And HDAC2
Tian Tu MD
Background: Keloid is a benign skin tumor with high recurrence rate after excision. Abnormal intracellular signaling is one of the key mechanisms. Over-activated phosphoinositide 3-kinase/serine-threonine protein kinase/mammalian target of Rapamycin (PI3K/Akt/ mTOR) signaling pathway and overproduction of histone deacetylases 2 (HDAC2) were also observed in keloid fibroblasts (KFs).
Objective: This study aimed to explore the possibility of reversing KF pathological phenotype using CUDC-907, a dual inhibitor of PI3K/Akt/mTOR pathway and HDACs.
Methods: KFs and keloid xenografts were treated with CUDC-907 to test its inhibitory effect on KF pathological activity in vitro and in vivo. CCK- 8 and cell cycle analysis were used to examine cell proliferation, whereas cell migration and invasion were analyzed with scratch assay, transwell and OrisTM migration and invasion assays. qPCR and Western blot were respectively used for gene and protein expression and H&E and immunohistochemical staining were employed to visualize the alteration of histological and related protein expression.
Results: CUDC-907 could inhibit cell proliferation, migration, invasion and ECM deposition of in vitro cultured KFs and also suppress collagen accumulation and disrupt capillaries of keloid explants ex vivo and in vivo. Mechanism study revealed cell cycle arrest at G2/M phase along with enhanced expression of p21 and decreased cyclin B expression. CUDC-907 not only inhibited AKT and mTOR phosphorylation and promoted acetylation of histone 3, but also significantly inhibited the phosphorylation level of Smad2/3 and Erk.
Conclusion: These preclinical evidences of its antikeloid roles suggested that CUDC-907 may become a potential targeted drug candidate for keloid systemic therapy.
Radiation Therapy 1
The Role of Adjuvant Radiotherapy for the Treatment of Keloids
Jonathan Tsao MD1
Keloids are a benign fibroproliferative disorder that is often associated with significant cosmetic impairment and local symptomatology. The risk of recurrence after local excision alone is high and the literature supports the role of postoperative adjuvant radiotherapy which significantly decreases this risk. The clinical procedure and the results of external x-ray, electron beam radiotherapy and brachytherapy will be examined and compared.
Topic Code: External Radiotherapy, Brachytherapy, Keloids
The Radiation Therapy In Keloids Treatment: A Comprehensive Review Of Pathomechanism, Damage Mechanisms And Cellular Response
Xiao Long, MD
Keloid management has always been frustrating and challenging. The combination therapy of surgical excision and radiation therapy was deemed as the last resort for decades. The authors performed a thorough and comprehensive review over the mechanisms on how radiation therapy damages the keloid cells. The keloid cells’ cellular response towards damage induced by irradiation was also studied based on original and current literatures. Mechanisms of damage generated by radiation therapy on keloid cells remained partially understood. However, direct damage was identified playing dominant role, in contrast to damage involved cancer cell apoptosis. Moreover, the p53 pathway and some inflammatory factors like interleukin-6 were believed to function in cellular response to irradiation. However, the transforming growth factor beta, which was the major dysregulated pathway involved in pathogenesis of keloid formation showed no apparent correlation with cellular response to irradiation damage. These pathways could partially explain radiation resistance in some refractory keloid lesions. The scientific basis and experimental proof in this field was still inadequate, which drove us to find more evidence to identify the key regulator response to damage engendered by radiation therapy. Further pathway identification may benefit the drug development to prevent keloid recurrence.
Primary Radiotherapy For Keloids: Optimal Time-Dose-Fraction For Maximal Resolution
Kamalendu Malaker 1,2,3, K Vijayraghavan4, Ian Hodson4, Twafic Alyaffi3, Mustafa Zaidi2, Rida Franka2
INTRODUCTION
Post-operative radiation following clean surgical excision is the only predictable successful treatment for keloids available. Standard dose fractionated radiotherapy for primary treatment so far has failed to achieve any acceptable regression and/or cosmesis. Rethinking of time dose fractionation of primary radiotherapy is very much needed.
RETHINKING
Keloids are tightly packed, hypoxic tissues, and are essentially biologically inert compared to its normal skin components. Keloids have been estimated to have high α/β ratio (10+). Therefore, classical fractionated radiotherapy, guided by “4R” principles, has failed to deliver reasonable response. A hypo-fractionated regimen of 750 cGy once per week for 5 weeks to a total dose of 3750 cGy has been used. The radiation response is by “Radiolysis” mostly and not on “4R” principle. Therefore, the adaptation of this “timedosed fractionation” has been successful.
RESULTS
Between 1977 and 2007, 97 keloids were treated. Ninetyseven percent (97%) had significant regression and cosmesis. Only three percent (3%) had partial response. Forty years of maximum and 10 years of minimum follow ups failed to report any cancer in this cohort.
RECOMMENDATION
Hypo-fractionated radiotherapy using 3750 cGy for five weeks, once every week, is recommended for primary radiotherapy of keloids.
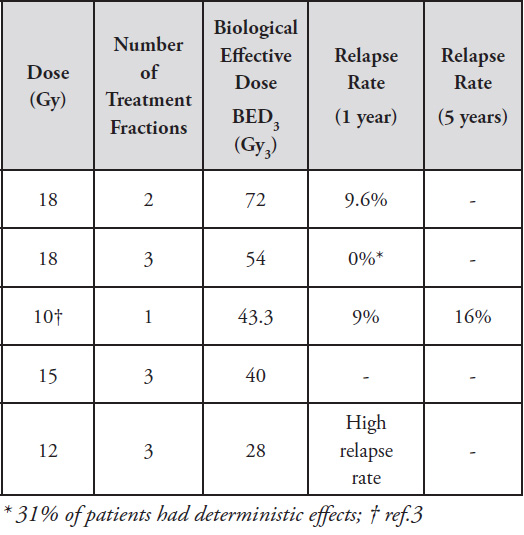
A Radiobiological Comparison Of Radiotherapy Treatment Regimes For Keloids And Its Implication For Treatment Protocols
Dr Henry Weatherburn (Head of Physics),PhD and Dr John Glees (Consultant Clinical Oncologist) MD, FRCR15
INTRODUCTION
A range of radiotherapy regimes for the treatment of keloids were presented at the 2nd International Conference on Keloids (ref.1). These varied not only in dose but also the number of treatment fractions employed in treatment delivery, the timing of these treatment fractions and the modality of their delivery, namely: superficial X-rays (100 – 160kVp); linear accelerator electron beams (6 or 7MeV); or brachytherapy (employing 192-Ir). While physical doses of radiation delivered by fractionated treatment can be added linearly, their resultant radiobiological effects cannot, so the current standard “linear quadratic” (LQ) model for calculation of radiobiological effective dose (ref.2) has been employed to determine the biological effective doses delivered by the various regimes. In turn this enables these to be compared using a “like for like” metric and, in turn, related to outcomes.
METHOD
The standard LQ model for biological effective dose (BED) can be expressed as follows: BED = n x d [1 + d / (ἀ / b)] where : n = number of fractions; d = dose per fraction (in Gray; Gy); ἀ / b = 3 for skin (2 for spinal cord; 10 for tumours, etc.)
Using this approach with ἀ / b = 3 for skin, the BED3 treatment doses (in Gy3) were calculated for a number of treatment regimes and related to outcome.
RESULTS
The comparative results for some sample regimes, considering dose only, can be presented as follows:
A further parameter not included is the issue of treating the patient within a specific timescale following surgical excision: this has been recommended as, ideally, 24 hours (with 48 hours acceptable) (ref.3), or a maximum of 72 hours (ref. 4). In the higher (physical) doses regimes reported above this was only true for the first treatment fraction and most had a week’s interval between the first and second (and, where scheduled, a third) fraction.
DISCUSSION & CONCLUSIONS
Addition ofphysical doses of radiation cannot be simplistically compared on a like for like basis for radiotherapy treatment and the LQ model has been used to demonstrate that higher physical doses delivered by multiple fraction treatments can have lower BED doses than a lower physical dose single fraction regime. However there is a confounding factor present which has not been accounted for in the above calculation , namely the lower biological response reported more than (at most) 72 hours after treatment. This would be present in later treatment fractions and such a factor is also present in the German DEGRO (ref.5) recommendations for radiotherapy treatment of keloids which recommend “a total dose ranging from 36 to 45 Gy using conventionally fractionated RT” A preliminary conclusion which can be postulated, in light of the BED of calculations, is that a single fraction dose of 10Gy is efficacious for keloid treatment and, if available, delivery by a superficial X-ray unit could be the most cost effective means of treatment delivery. However a further and more detailed international audit of results for treatment by different modalities, at various body sites and a review of aspects of the LQ model is desirable to reach more definitive conclusions about dose and fractionation to establish definitive treatment protocols.
REFERENCES
- Proceedings of the 2nd International Keloid Symposium at Pontificia Universita San Tommasso D’Aquino, Rome, Italy – June 7-8, 2018
- 21 years of Biologically Effective Dose. Fowler JF. The British Journal of Radiology, 83 (2010): 554–568
- Treatment of Keloids by Surgical Excision and immediate Postoperative Single-fraction Radiotherapy. Ragoowansi, R et al., Plastic and Reconstruct Surgery. (2003); 111: 1853-1859
- Adjuvant single-fraction radiotherapy is safe and effective for intractable keloids. Song C, Wu HG, Chang H, Kim IH & Ha SW Journal of Radiaiton Research, 55(5), 1 Sept 2014: 912 – 916
- DEGRO guidelines for the radiotherapy of non-malignant disorders Part III: Hyperproliferative disorders. Seegenschmiedt MH, Micke O, Niewald M, Mücke R,·Eich HT, Kriz J & Heyd R The German Cooperative Group on Radiotherapy of Benign Diseases (GCG-BD) Strahlenther Onkol (2015) 191:541–548
- Radiation therapy for the Adjunctive Treatment of Surgically Excised Keloids: a Review Cheragi, N, Cognetts A, and Goldberg D J, Clinc Aesthet Dermatolog (2017); 10 (8): 12-18
Estimates of Radiation Risks Arising from the Treatment of Keloids by Radiotherapy
Dr Henry Weatherburn (Head of Physics), PhD1, Dr John Glees (Consultant Clinical Oncologist) MD, FRCR1, and Prof Kamal Malaker (Director of Clinical Oncology, CCEC) MD, PhD, FRCS2
INTRODUCTION
Quantitative estimates of the risk of side effects arising from the treatment of keloids by radiotherapy are important. These are determined both for excised and unresected keloid treatment regimes, particularly the risk of skin cancer induction.
METHOD
For excised Keloids a standard treatment is the delivery of a dose of 10Gy in a single treatment fraction using a 60kV (or sometimes higher kV) X-ray beam or, alternatively, an electron beam. For unresected Keloids, two regimens are often employed: either a total of 16Gy given in four quarterly fractions over a period of a year; or 37.5Gy given in five once weekly fractions (ref.1; ref.2).
As ionising radiation is employed in this treatment, deterministic effects arise, both as acute effects, such as erythema, etc. and late effects, such as pigment changes, etc. A risk of stochastic effects, primarily skin cancer, is also present and a quantitative estimate of this risk is derived from radiobiological risk calculations and compared with risks reported in reviews.
To estimate the risk of skin cancer, calculations are undertaken for the treatment regimes described above noting that, if two or three keloids are irradiated, the risk will then be double or tripled.
An irradiated area of 20 cm2 is assumed and it will also be assumed that the surrounding site is protected by the lead applicator, with the remainder of the body receiving only minimal leakage and scattered radiation. Time gaps between treatment fractions are also ignored, and , in the first instance, the effect of age. In calculating the risk initially only the skin is taken into account and other underlying irradiated tissues are ignored. The calculation assumes a standard middle-aged adult (ref. 3).
RESULTS:
The total body skin area is assumed to be 2 m² and, assuming that the radiation is relatively superficially absorbed and the area of the keloid and the surrounding planned treatment margin only being exposed, 20 cm² of skin is thus exposed with 10 Gy. Using WR = 1 for x-rays and WT = 0.01 for skin, we obtain an effective dose to the irradiated skin of 0.1 mSv. For a patient having unresected three unresected keloids treated each with a dose of 37.5Gy this could rise to 1.13mSv (with a radiation risk coefficient of 0.01%) and can be compared with the effective dose for annual background radiation which, for the UK is approx 2.6mSv.
Extending this model to various organs, muscles, bones, and bone marrow (e.g. for radiotherapy of a heel spur employing 200 kV x-rays, dose 12 Gy, area 80 cm²), where an effective dose for skin has been estimated to be 2.9 mSv, and, including all organs, this increases to 8 – 9.5 mSv, i.e. by a factor of approx. three (ref. 4). The risk also increases by a factor of three at age 25 compared with age 50 and for women is double that for men.
DISCUSSION & CONCLUSIONS:
Overall the risk arising from the treatment of large areas of skin with sensitive underlying tissue, e.g. mammary tissue in the breast, may increase risk of cancer induction to 0.1% – 1% and may explain a reported case of potentially radiation induced breast cancer (ref.5).
Induced cancers reported in reviews of keloid treatment are at magnitudes of below 1 in 1,000 (i.e. < 0.1%), or as low as 1 in 10,000 (i.e. <0.01%), which show a general correspondence with the above values (ref.1, ref.6 & ref.7).
REFERENCES
- Treatment of Keloids by Surgical Excision and immediate Postoperative Single-fraction Radiotherapy. Ragoowansi, R et al., Plastic and Reconstruct Surgery. (2003); 111: 1853-1859
- Retrospective Analysis of Treatment of Unresectable Keloids with Primary Radiation Over 25 Years. Malaker, K et al., Clinical Oncology (2004); 16: 290 – 298
- Annals of the ICRP Publication 103. The 2007 Recommendations of the International Commission on Radiological Protection Editor J. VALENTIN, Elsevier (2017)
- Estimation of the carcinogenic risk of benign diseases from shoulder to heel. Jansen J, Boerse J, et al, Radiotherapy and Oncology (2005); 76: 270 – 277
- The risks of treating keloids with radiotherapy. Botwood, N, et al. British Journal of Radiology (1999); 72: 1222 – 1224
- Is radiation therapy for keloids acceptable? The risk of long term carcinogenesis. Ogawa R, Myashita T et al, Plast Reconstr. Sirg. (2009); 124:1196 – 1201
- Radiation therapy for the Adjunctive Treatment of Surgically Excised Keloids: a Review Cheragi, N, Cognetts A, and Goldberg D J, Clinc Aesthet Dermatolog (2017); 10 (8): 12-18
A Novel Treatment Of Keloids: Micro-Plasma Radio-Frequency Combined With Hypofractionated Electron-Beam Radiation
Zhifei Liu, MD
Background: Micro-plasma radio-frequency (MPR) technology has been demonstrated a safe and effective treatment of kinds of scars.
Aims: We assumed that combining MPR technology with hypofractionated electron-beam radiation therapy can not only show excellent therapeutic effect on keloids but also decrease the recurrence rate.
Methods: 22 Asian patients (16 males, 6 females, ages 19-46 years, mean age 28.14±7.31 years) with keloids over half a year and Fitzpatrick skin types IIIVI were enrolled in this study. All patients received a single MPR technology treatment by roller tip at 80- 100 watt, and then hypofractionated electron-beam radiation of 6 MeV were performed twice, within 24 hours and one week after the operation, with 9 Gy per time. Improvement were determined by the Vancouver Scar Scales (VSS) according to digital photographs.
Results: The results show that the volume of keloids reduced significantly among most patients. Roughly 95.4% patients were basically content with the treatment based on the improvement of scars. The mean grade of pain on first day after treatment was 6.41±1.27. 3 patients encountered with mild to moderate hyperpigmentation , and none of malignance and worsening or recurrence of scars was observed. Collagen remodeling and increased new collagen deposition were seen 3 months after treatment based on the histologic examinations of biopsied tissue.
Limitations: Patients (age <12 years, radiosensitive locations: breasts or thyroid) are not applicable to this method, and not all hospitals are equipped with the linear accelerator. It is difficult to achieve a good effectt if the height of keloids is higher than 1cm.
Conclusions: MPR technology is an effective method for the keloids with minimal complications, and can decrease the recurrence rate combined with post-operative hypofractionated electron-beam radiation therapy.
Pathogenesis of Keloid Disorder
Extracellular Matrix Gene Expression Profile In Keloid Fibroblasts: The Effects Of Cellular Stretching
Shan Wang1,2, Edward Macarack1, Jie Yang2, Joel Rosenbloom1, Jouni Uitto1
Keloids, benign cutaneous tumors whose development is frequently elicited by trauma, are composed of the extracellular matrix, primarily collagen. Previous studies by us have demonstrated that collagens type I and III are the major components, but type VI collagen gene expression is activated particularly at the early stages of keloid fibrogenesis. While the activation of collagen gene expression has been shown to take place at pre-translational level, the mechanisms of activation of gene expression are largely unknown. In this study, we have examined extracellular matrix gene expression by quantitative PCR in keloid fibroblasts, in comparison to fibroblasts obtained from unrelated healthy controls. The results confirmed activation of collagen I and III gene expression in keloids, and revealed the abundance of different fibronectin mRNA splice variants (Fn-C5, Fn-EDA and Fn- MID). Fibroblasts stretched at a strain of 10 percent at frequency of 1 Hz demonstrated marked increases in mRNA transcript levels in keloid fibroblasts, particularly showing elevated mRNA for total fibronectin and its splice variants as well as for integrins α4, α5, α9 and β1. Furthermore, activation of the gene expression in many cases was significantly higher upon stretching of keloid fibroblasts as compared to control cells. Collectively, our results demonstrate that expression of certain extracellular matrix genes is activated in cultured keloid fibroblasts as compared to controls, and such changes are markedly accentuated by stretching of the cells, emphasizing the role of the extracellular milieu in selectively controlling the gene expression profile as a contributor to keloid formation.
Keloid Is Not Scar: The Immune Microenvironment Evidences
Youbin Wang, MD
In general,keloid extend or originate beyond the confines of the original lesion and do not regress. Keloids may be uncomfortable or itchy, and may be much larger than the original wound.However, the formation of physiology scars is a part of wound healing. Although there are some similiar symptomes between keloid and physiology scars such as red and swollen, physiology scars can be self-limited and turn into pale and smooth in a several months. Some researched have analyzed the differences between keloid and physiology scar from many standpoints. However, the differences in immune microenvioronment between keloid and physiology were never been found. Via using Oncomine Immune Resoinse Research Assay, we measured the expression of microenvironment genes involved in tumorimmune system and inflammatory signaling pathway in keloid and physiology scar. 20 different genes was marked. Indicating that keloid and physiology scar are different in immune microenvironment factors.
Reconstructed Human Keloid Model Show Heterogenety within Keloid Scars
Grace C. Limandjaja1, Leonarda J. van den Broek1, Melanie Breetveld1, Taco Waaijman1, Stan Monstrey2, Rik J. Scheper3, Frank B. Niessen4, Susan Gibbs*,1,5
Keloid scars are ofteh described as having an actively growing peripheral margin with a regressing centre. The aim of this study was to examine the possible heterogeneity within keloids and the involvement of different regions within and around keloid scars in the pathogenesis, using an in vitro keloid scar model. In vitro skin models were constructed from keratinocytes and fibroblasts from normal skin and different regions within and aroun keloid scars: periphery, centre, and (adjacent) surrounding-normal-skin regions. Additionally, fibroblasts were central keratinocytes. All keloid regions showed increased dermal thickness (trend) and increased contraction compared to normal skin models, particularlyin central regions. Myofibroblasts were present in all keloid regions but were more abundant in models containing centraldeep keloid fibroblasts. Secretion of anti-fibrotic HGF and extracellular matrix collagen IV gene expression showed differential expression between keloid and normal skin. Distinct trends showing differences between peripheral and central regions within keloids were observed for inflammatory cytokine CCL20, CCL27, CXCL8, IL-6 and IL-18 secretion. Parameters for surrounding-normal-skin showed similarities to both non-lesional normal skin and keloids. In conclusion, a simple but elegan method of culturing keloid-derived keratinocytes and fibroblasts in an organotypic 3D scar model was developed, for the dual purpose of studying the underlying pathology and ultimately testing new therapeutics. In this study, these tissue engineered scar models show that the central keloid region shows a more aggressive keloid scar phenotype than the periphery, and that the surrounding-normal-skin also shares certain abnormalities characteristic for keloids.
Non-Surgical Management of Keloid Lesions
The Establishment Of Keloid Comprehensive Diagnosis And Treatment System: Treatment Experience Of Non-Operative Treatment
Wen Yun Ting, MD
Some keloids, after evaluated by the Keloid Comprehensive Diagnosis and Treatment System, are not suitable for surgery. High suturing tension after excision of these keloids with large and/or multiple lesions could lead to high recurrence rate. Under this condition, non-surgical treatment is considered. Besides, nonsurgical treatment is good for thin keloids which could be controlled by glucocorticoid with dye laser therapy. If the evaluation scale indicates a bad prognosis or certain symptoms recur, micro-PSR with positron soft-tissue irradiation are considered when a keloid is soft and less than 4mm thick. After the wound is fully recovered, dye laser is administrated to improve vasoconstriction. If possible, injection of Botox onto the lesion and surrounding muscles could further release tension and reduce sebaceous glandes secretion. For those with high aesthetic requirements, superficial fractional laser could be administrated in the early stage to repair the outlook, so as to prevent the keloids from relapse as well as improve their appearance.
Re-Thinking The Medical Management Of Keloids: Reflections And Experiences From A Busy Urban Clinical Practice In Kingston, Jamaica.
Dr. Patricia Yap B.Sc. MB.BS. Dip. Derm.1, Dr. Jonathan Ho MB.BS., Dr.Sc. Dip. Dermpath2, and Prof. Kevin A, Fenton MB.BS. (Hons) M.Sc. Ph.D. FFPH3
Corresponding Author: Dr Patricia Yap.
Email: patyapja@gmail.com
INTRODUCTION
Keloids are nodular, firm, tender, movable, nonencapsulated masses of hyperplastic scar tissue, occurring in the dermis and adjacent subcutaneous tissue, usually after trauma, surgery, burns, or severe cutaneous disease such as cystic acne. Traditional treatments have largely relied on combinations of surgery, radiotherapy, chemotherapy and cryotherapy, in part reflecting the historic view of keloids as benign tumours. These treatments have relatively poor outcomes, often complicated by keloid regrowth after repeated attempts at removal. Medical management of keloids remains underutilized, so too has the use of medical treatments to prevent recurrence.
This presentation reviews the experiences of three patients that benefitted from medical treatment of confirmed keloids, all managed by Dr. Patricia Yap in her clinical practice in Kingston Jamaica. We introduce the application and results of a novel topical treatment option which demonstrates objective improvements in clinical outcomes (reductions in the size, appearance and recurrence of keloids) with enhanced patient satisfaction.
BACKGROUND
In 2002, a middle-aged female patient attended Dr. Yap’s practice for a consultation regarding multiple keloids on her back. At this time, the typical treatment would have been the painful, uncomfortable intralesional steroid treatment. Each and every keloid would have had to be injected, therefore, the volume of Triamcinolone Acetonide (TA) solution would result in systemic side effects. The patient suggested that there should be a cream (topical treatment). With this suggestion, Dr. Yap who has a first degree in chemistry, created a unique delivery system that allowed the introduction of the steroid into the dermis topically.
On commencing treatment, the decision was taken to not to use intralesional steroids on the entire back as it would have incurred side effects. Consequently, a half back approach to application was implemented.
On the left of the patient’s back, intralesional steroids along with topical therapy was used, whereas on the right side, only the topical therapy was used. The keloids on both sides decreased in thickness, even though the left side progressed much faster. The patient experienced little-to-no systematic side effects and the outcomes (Figure 1.) were satisfactory for the patient with significant reduction in reported pain, itchiness, and growth.
Figure 1. Before and after images of Patient A. Female. Kingston, Jamaica
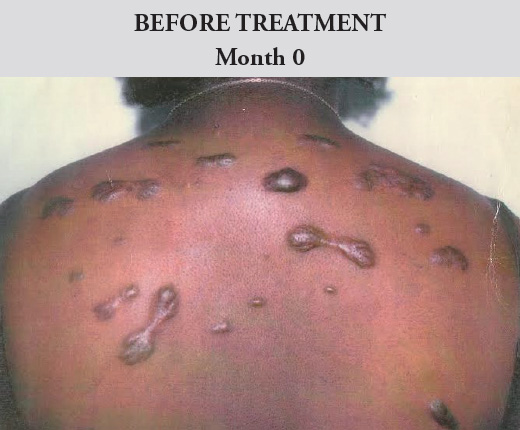
Treatment applied: Left Back – Intralesional and Topical Therapy. Right Back – Topical Therapy only
Following this initial positive response, Dr Yap has refined and expanded the application of topical treatment for patients with keloids over the past seventeen years. The following case studies present 3 cases which demonstrate the success of topical treatments alongside or instead of intralesional injections.
CASE STUDIES
In the three cases below and pictures that follow, it is evident that using a novel topical treatment option is beneficial to the patient. This not only gives control back to the patient but also results in decreasing the burden in the healthcare system.
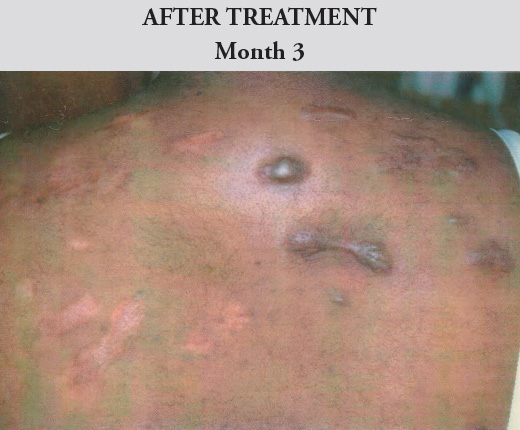
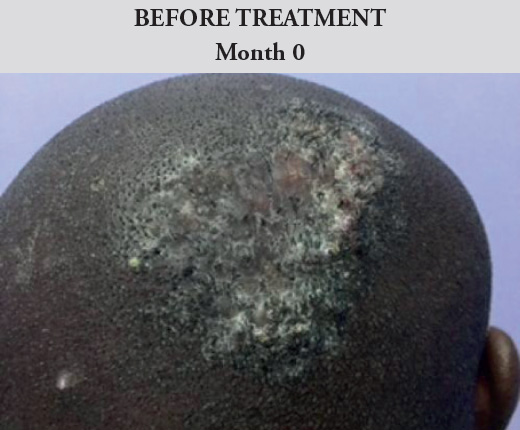
Case 1: Combination therapy using topical and standard intralesional steroids Male, 35 years old, presented with extensive folliculitis keloidalis on the scalp involving the crown and the back of the head.
The patient was diagnosed with both folliculitis keloidalis on the crown of the head and folliculitis keoidalis nuchae at the back of the head (occipital area). For the former, the patient was applied the topical treatment only for one month. The folliculitis keloidalis of the crown resolved completely after this period (see Figure 2a).
For management of the folliculitis keloidalis nuchae, the patient was prescribed both intralesional and topical treatments. The intralesional steroid was given at the end of the first and second months of treatment to the folliculitis keloidalis nuchae. The third month only topical treatment was used. The resolution over the 3 month period is shown in Figure 2b.
Figure 2a. Before and after images of Case 1. Male. Aged 35. Kingston, Jamaica

Diagnosis: Folliculitis keloidalis. Treatment applied: Topical therapy for 1 month only
Figure 2b. Before and after images of Case 1. Male. Aged 35. Kingston, Jamaica


Treatment applied: Topical treatment for 3 months, supported by intralesional steroids at the end of Months 1 and 2.
Case 2: Topical treatment post-surgerical keloid scars
Female, 32 years old, with past history of keloids on chest and shoulder from minor injuries. After having developed keloid scars after her first cesarean section, the patient requested post-op treatment for her second cesarean section to prevent keloid recurrence. At two weeks post-op care, the patient’s keloid already started to develop, shown on the right. The topical treatment was then applied for two weeks which resulted in 100% flattening.
Figure 2. Before and after images of Case 2. Female. Aged 32 years. Kingston, Jamaica


Treatment applied: Topical therapy only.
Case 3: Topical treatment monotherapy
Female, 67 years old, referred from a general practitioner with chronic itching and spontaneous keloid formation on chest for the past nine years.
This patient developed multiple keloids on her chest from scratching. The increased irritation caused loss of sleep and general discomfort. After one month of receiving the novel topical treatment, the patient was no longer uncomfortable and the keloids were flattened
Figure 3. Before and after images of Case 3. Female. Aged 67. Kingston, Jamaica


Treatment applied: Topical Therapy only
CONCLUSIONS
These three cases are illustrative of the very positive treatment outcomes for keloids being achieved with medical treatment (topical applications) in Dr. Yap’s clinical practice for the past seventeen years. Unfortunately, when the patients are satisfied with the outcome, whether due to the decrease in pain, itchiness and size they often do not return to the clinic for the final picture. Further, more robust clinical studies are now planned to systematically study and document patient outcomes and improvements in patient experience.
However, from these documented case studies and clinical experience, it is evident that self-applied therapeutics can minimize healthcare burden by promoting self-treatment rather than intensive inoffice treatment. The ability to self-manage with topical preparations also encourages early treatment to prevent future recurrence of keloids. They may therefore form the basis for effective first-line therapy for the medical treatment of keloids.
Microneedle-based Skin Patch for Pathological Scars Treatment
Chenjie Xu*1, David Yeo1, Xiaoyu Ning1, David Ian Leavesley2, Hongliang Tey3
* Email correspondence to: CJXU@ntu.edu.sg
Key Words: microneedles, transdermal drug delivery, abnormal scar
Background: Keloid tissue shows increased dermal thickness and are composed of thick scar tissue, the result of an over-production of collagen. Current treatment for keloids include the antitumor/ antimetabolite drugs, steroid drugs, peptide/protein, RNA, and stem cells. These are currently delivered through oral administration, intralesional injection, or topical application. However, oral administration is unsuitable for peptide, RNA and stem cells, while intralesional injection is painful and limited to small areas. Topical delivery is preferred by patients, is easy to apply for any size of keloid, and most therapeutics can be formulated for topical delivery – with the exception of interventions unable to permeate through fibrous scar tissue. The microneedle platform can be used to deliver small molecules, peptide, RNA, and stem cells etc.
Method: We have developed microneedle-based skin patches to faciliate the delivery of therapeutics through the epidermis and directly into hyalinsed keloidal tissue. The devices are made from biodegradable polymers within which therapeutics may be pre-embeded. Once inserted into keloid, the tips of microneedles slowly degrade, release and deliver the encapsulated therapeutic. The devices have been characterised for mechanical properties, inhibition of keloid-derived fibroblast proliferation and collagen secretion, and for effectiveness in the rabbit ear scar model.
Results: The microneedles were shown to penetrate skin tissue. Keloid-derived fibroblasts cultivated in 2D did not exhibit any significant change in cell death when exposed to the microneedle device. However, after 12-hours of expose to the microneedle patch, cell death increased from 5.43±1.12% to 83.8±12.0%. In rabbit ear hypertrophic scar model, control wounds without the presence of patches generated regions of raised dermis originating from the wound site (3/3); wounds treated with microneedle patchesresulted in dermis tissue thickening in 83.33% of the wounds (15/18).
Conclusion: Microneedle skin patch is an effective platform to reduce the growth of keloids. It has potential for painless transdermal delivery of therapeutic agents into scar tissue. Its versatility permits the delivery of various kinds of therapeutics including small molecules, peptide, RNA and stem cells etc for the management of keloidal collagen. Funding Sources: NTU-Northwestern Institute for Nanomedicine; Singapore A*Star Biomedical Research Council (IAF-PP grant); Primary Research & Development Plan of Jiangsu Province of China (BE2016770).
REFERENCE:
- Shiying Liu, David C Yeo, Christian Wiraja, HongLiang Tey, Milan Mrksich, Chenjie Xu*. Peptide delivery with poly(ethylene glycol) diacrylate microneedles through swelling effect. Bioengineering & Translational Medicine. 2017 2(3): 258-267. doi: 10.1002/btm2.10070
- David Yeo, Elizabeth Balmayor, Jan-Thorsten Schantz, Chenjie Xu*. Microneedle Physical Contact as a Therapeutic for Abnormal Scars. European Journal of Medical Research. 2017, 22(1): 28. doi: 10.1186/s40001-017-0269-6.
- Xue P, Yeo DCL, Chuah YJ, Kang YJ, Xu CJ*. Drug-eluting Microneedles for the Self-management of Keloids. Technology. 2014; 2(2): 144-152. doi: 10.1142/S2339547814500137
A Case Of Earlobe Keloid Regression By Bottom Ligature And Injection With Corticosteroid And 5-FU
XiQiao Wang, MD1
A 34-year-old girl suffered from earlobe keloid for 6 years after puncture of ear ring. 2 years ago, she received a corticosteroid injection for 6 times, it had a little reduction. After 6months, it recurred with more larger size about 1.5*1.5*1.2cm. This time, we use the silk ligatured at the bottom of keloid, persisted for 23-24hs each day , and injected with corticosteroid and 5-FU each month at the bottom and entity. After 4 months, the bottom became more and more thin, and the entity became purple and then undergo drying necrosis , 1 month later, the necrotic entity fall off at the bottom, almost without wound. Thereafter, treated with 3 injections, the keloid completely resolved. Conclusion The bottom ligature could reduce the blood supply, cause the entity necrosis, and accelerate the keloid regression on the base of injection of corticosteroid and 5-Fu.
Role Of Cryotherapy In Treatment Of Bulky Keloids
Michael H. Tirgan, MD
INTRODUCTION
Usage of contact cryotherapy in treatment of keloids dates back to 1950 [1]. There are numerous references about efficacy of cryotherapy in treatment of keloids [2,3]. Like any other medical procedure, contact cryotherapy should be delivered properly in order to achieve optimal results. Materials that are needed to apply cryotherapy are:
- Liquid nitrogen
- Properly sized cotton swab
For keloids that are few millimeters in diameter, the readily available cotton swabs (Figure 1) can be used.
For keloids that are larger than one centimeter, the author custom makes his own swabs by rolling a nonwoven medical gauze and inserting one end of the rolled gauze inside a 10 ml test tube. The exposed end of the gauze is then cut with scissors to achieve a flat tip surface (Figure 2).

Figure 1. Commercially available cotton swab being used to apply cryotherapy to a small ear keloid.

Figure 2. Custom made large cotton swab being used during the application of cryotherapy to a large ear keloid. The frozen keloid appears white.
Cryotherapy For Treatment Of Ear Keloids
The best treatment results with cryotherapy are achieve in patients with ear keloids. With repeated cycles of cryotherapy almost all ear keloids, no matter how small or how large they may be, can be successfully removed.
The purpose of using cryotherapy as the first-line treatment for ear keloids is to avoid the risks associated with surgery and adjuvant radiation therapy [4, 5]. As opposed to surgery, that carries a well-known risk for worsening of the keloid lesions, cryotherapy does not pose such a risk. Indeed, there are no published reports to even indicate such a causal association. Successful treatment of keloids with cryotherapy requires patience and perseverance, both from the treating physician as well as the patient. Both parties need to commit to repeated cycles of treatment on a regular basis. Cryotherapy shall be repeated until all protruding components of the keloid are removed. Pain Control
Cryotherapy is a painful procedure. Pain starts immediately after the application of liquid nitrogen and can last for 24-48 hours. The smaller the keloid is, the less pain there will be during and after the procedure. Application of cryotherapy to large, semimassive and massive keloids can be quite painful, and without taking proper measures, the procedure cannot be completed as planned. Pain control is the most important factor in achieving success with cryotherapy. Poor pain control will result in lack of compliance and interrupted treatment cycles.
REFERENCES
- Allington HV, Liquid nitrogen in the treatment of skin diseases. Calif Med. 1950 Mar;72(3):153-5.
- Muti E, Ponzio E. Cryotherapy in the treatment of keloids. Ann Plast Surg. 1983 Sep;11(3):227-32.
- Rusciani L, Rossi G, Bono. Use of cryotherapy in the treatment of keloids. R J Dermatol Surg Oncol. 1993 Jun;19(6):529-34.
- Miyahara H1, Sato T, Yoshino K. Radiation-induced cancers of the head and neck region. Acta Otolaryngol Suppl. 1998;533:60-4.
- Ron E. Cancer risks from medical radiation. Health Phys. 2003 Jul;85(1):47-59.
Abstract Presentations
Conducting Clinical Trials In Keloid Disease Research – Ethical And Study Design Considerations
Patricia L. Danielsen
Keloid research is not only suffering lack of clinical studies but ethical and study design challenges may often lead investigators no other opportunities than to down scale on study design, follow-up time and outcome measures. This talk will from the researcher’s own clinical and experimental experience on two continents share with the audience the legal, investigative and methodological demands and sometimes even obstacles they will probably meet when aspiring to conduct the perfect clinical keloid study.
What Is The Best Approach To Deal With Keloid Scars ?
Raul Caceres, MD
For the last 40 years all of us have tried several options to come up with an optimal result to benefit patients with keloids. During my training in general surgery and plastic surgery I became interested in burn patients. In a 2 year fellowship at Johns Hopkins in Baltimore, Maryland and later as a Director of the Burn Unit at Harlem Hospital in New York City my main approach was always surgical first, in combination with several other modalities.
Three years ago I met Dr. Michael Tirgan and referred him a patient with large keloids in both ear lobes. Upon seeing my patient after 6 months, I was very impressed with the outcome and equally important the psychological improvement of this young girl.
As a result I believe that the non-surgical approach first is better. Thanks to the Keloid Research Foundation and the vision of Dr. Tirgan to come up with a unified front and a world-wide collection of data, we could improve the outcome as well as the satisfaction of our patients.
In Oruro, Bolivia where I was born there was a great need of a burn unit for indigent children. I with donations built a burn unit similar to the ones in the US. Last year Dr. Tirgan and I were there for a medical congress and decided to start an office of The KRF to collect data with Dr. Tirgans protocol. I was very happy to attend the Rome meeting and have the opportunity to meet some of you and I believe all of us are capable to achieve better results for the benefit of our patients.
Single Surgeon’s Experience With Keloids In India Over 3 Years
Kannan Prema, MD
Keloid is a fibroproliferative skin disorder occurring probably following trivial trauma in genetically susceptible population , producing significant cosmetic and functional disabilities, with no definitive cure. The patients present to us with clinical complaints of unsightly scar with pruritis, pain due to surrounding tissue contraction, inflammation and wound at the midline of the scar, and suspicion of carcinoma. The keloid scar is a social stigma for men and women with significant psychological impact, affecting their personal and social life. There is no single best therapeutic modality for all keloids. The methods of treatment used in our institution over a period of three years , January 2016 to December 2018 , was based on the number of keloids, location, size, associated clinical factors, condition of the surrounding tissues, comorbid conditions of the patient and previous treatment for the keloid scar. The chosen treatment modalities were scar gel silicone sheet, surgery , radiotherapy, triamcinolone injection. The therapies were named as Singleton – scar gel silicone gel sheet, Double Decker – triamcinolone injection with scar gel silicone gel sheet, Sandwich – Surgery with radiotherapy and scar gel silicone gel sheet combo. The results were reliable and reproducible. We are working on Quadra, Penta, Hexa and finally The Rainbow therapy…
Lasers In Treating Keloid Lesions: Can The Treatment Be Harmful To Some Patients? Results Of An Online Survey
Michael H. Tirgan, MD
Background: Lasers are among the most commonly used tools in day to day practice of dermatology. Although there are several reports about the utility and efficacy of laser treatment in keloid lesions, there is a paucity of literature as to how keloid patients perceive the efficacy of this modality.
Objective: To assess patients’ perception of the efficacy of lasers in treatment of keloid lesions. Material and methods: The underlying survey study was approved by the Institutional Review Board (IRB). An online keloid survey was launched in November 2011. Participants were asked to provide answers to numerous questions about their keloid disorder, including their perception of the efficacy of laser for treatment of their keloidal lesions. Descriptive statistics are provided.
Results: As of November 20, 2017, total of 1597 individuals participated in this survey. 191 participants indicated that they had previously received at least one laser treatment for their keloids, among whom 174 provided an assessment of the benefit of this intervention. Five patients (2.9 %) reported that laser treatment cured their keloids. 47 patients (27%) reported having benefited from the treatment. 82 patients (47.1%) reported no improvements, but most interestingly, 40 patients (23%) reported that laser treatment caused worsening of their keloids.
Conclusions and Relevance: With several limitations, this study represents the first step in developing a patient-reported measure of treatment success and benefit drawn from laser treatment. The most important finding of this study is that 23% of patients reported worsening of their keloids with this treatment. Worsening of keloids after laser treatments has never been reported.
Radiation Therapy 2
Treatment Of Keloids With Corticosteroid Injection Alone Or Combined With Surgical Excision Compared With Ionizing Radiation And Other Therapies: A Systematic Review And Meta-Analysis Of Randomized Controlled Trials
Patricia L. Danielsen, Wang Ru, Magnus S. Ågren, Janine M. Duke, Fiona Wood, Xiao Xi Zeng, Yu Mao, Ying Cen
The justification for management of keloid scars with corticosteroid therapy or ionizing radiation (radiotherapy) alone or combined with surgery remains debatable. The aim of this systematic review and meta-analysis of randomized controlled trials (RCTs) was to assess the effects of intralesional corticosteroid injection in treating keloids or preventing their recurrence after surgical excision. Searches for RCTs were conducted through the Medline, Embase, EBSCO and Cochrane databases from 1974 to 2017. Two authors independently reviewed study eligibility and assessments, extracted data, analyzed the results and assessed methodological quality. After screening the literature, 16 RCTs conducted in ten countries on 855 patients aged from 10 to 68 years were scrutinized. In 10 RCTs, corticosteroid intralesional injections were compared with 5-fluorouracil, radiotherapy, etanercept, cryosurgery, botulinum toxin type A and topical glucocorticosteroid under silicone dressing. Corticosteroid intralesional injections were more effective than radiotherapy but equipotent with the other interventions. In conjunction with keloid excision, corticosteroid treatment was compared with radiotherapy, interferon α-2b and the calcium channel blocker verapamil. Two RCTs demonstrated fewer keloid recurrences with adjuvant radiotherapy compared with corticosteroid injections (RR 0.43, 95% CI: 0.21 to 0.89) although complications were more common with adjuvant radiotherapy. More high quality, multicentre, large scale RCTs are required to establish the effectiveness of corticosteroids and radiotherapy in keloid management.
Treating Keloids With Adjuvant High-Dose Rate Brachytherapy
Jonathan Tsao MD1, Sarah Rauth MD, Jasper Yuen MD, Kailin Lawrence MRTT, Gwen Bond RN, Eric Sabondjian CCPM
The role of postoperative adjuvant radiotherapy for keloids in decreasing the risk of recurrence has been supported by clinical literature. Although less commonly employed than external beam radiation adjuvant brachytherapy is a promising treatment modality. This institutional retrospective review analyzed the clinical results for 27 patients with 39 keloids treated over the last 3.5 years with surgical excision and postoperative HDR brachytherapy. The patients ranged in age from 19 to 78 years and there were 8 males and 19 females. All patients were treated to a dose of 18 Gy in 3 fractions at a depth of 0.5 cm. within 36 hours following excision. Median follow up was 16 months and median active treatment length was 7.3 cm. There was no case of recurrence but there were 4 cases of transient hyperpigmentation, 5 cases of wound dehiscence, and one case of infection. These early clinical results support the effectiveness of this treatment.
Topic Code: Brachytherapy, Keloids
Role of radiation therapy in the treatment of keloid lesions. Experience of Peking Union Medical College Hospital
Jie Shen, MD
We aimed to analyze the outcomes of hypofractionated high-energy electron beam radiotherapy for the treatment of keloids. From February 1998 to January 2012, 568 patients with a total of 834 keloids underwent radiotherapy: 826 lesions with postoperative radiotherapy, and 36 with skin-grafting. Lesion size was >5 cm in 335 keloids. An electron-beam of 6 or 7 MeV was used, with a total dose of 18 Gy (two fractions with a 1-week interval) covering the lesion with a 1-cm margin. The time between surgery and radiotherapy was 24–48 h. Skin-grafted patients underwent radiotherapy 10–15 days after the operation. The median followup was 40 months (range: 12–160 months). The local control rate was 88.25% (736/834). The relapse rate was 9.59% (80/834), and the time to relapse was 6–28 months (median: 12 months). Univariate analyses showed that gender, age, keloid size, keloid site, skin grafting, and operation-to-irradiation interval influenced the local control rate. Multivariate analysis showed that the relapse rate was correlated with gender (P = 0.048), age (P < 0.01), operation-to-irradiation interval (P < 0.01), keloid site (P < 0.01), surgical method (P = 0.04) and keloid size (P < 0.02). Adverse effects were observed in 9.83% (82/834). No radiationinduced cancers were observed. Hypo-fractionated high-energy electron beam radiotherapy for keloids yielded excellent outcomes, especially in cases without skin grafting. Early postoperative radiotherapy with limited hypofractionation could be a good choice for keloid treatment.
Ten Years Of Experience With Superficial Radiation Therapy In The Treatment Of Keloids At The University Of Nairobi. Outcome And Lessons Learned
Ferdinand Nangole, MD1
Keloids are prone to recurrence . surgical intervention without adjuvant therapy of either radiotherapy or steroid injection results in a recurrence of almost 100 percent . The role of radiotherapy in the management of keloids disease is now well established with different centres recording different recurrence rate . we share our experience in the management of keloids in the last 10 years with the use of 12 grays one shot external radiation. A total of 523 patients were managed with superficial radiotherapy in our series. The age ranges for the patients was 18years to 70 years with a mean age of 39 years. Majority of the keloids managed , were ear lobe keloids contributing to 45 percent of the keloids managed followed by the anterior chest wall and abdominal keloids . Our overall 10 year recurrence rate was less than 10 percent No long term complications were noted in all our patients and majoirity were happy with the overall outcome .
In conclusion supefcial radiktherapy post surgery offers one of the best results in in the management of patienst with keloids with minimal recurrence. This modlaty of treatment is associated with minimal complication and probably has the lowest recurrence rate.
Discussion of four unusual cases of Keloid tumours
John Glees MD
Dr John Glees will present 4 unusual cases of Keloid tumours each seen at time of referral to Dr Glees. This will take the form of a clinical presentation of each case illustrated with photographs of each of the four cases. John will then present various possible treatment options for each case in the form of bullet points. Each bullet point is up for discussion by the audience. Then a vote will be taken by a show of hands which of the options is considered the most appropriate.
Then John will disclose to the audience which of the treatment options was indeed undertaken again illustrated with photographs showing long term results wherever possible.
This presentation will give a better understanding as to the role of radiation treatment in the management of Keloid tumours. Sometimes we recommend superficial radiation, at other times we use high energy photons (machine produced X-Rays) or Electrons (negative particle irradiation), also machine produced, where a direct field is used to give a uniform dose to a particular depth of tissue or thickness of Keloid. The concept of Bolus explained.
The role & delivery of these different types of radiation will be discussed. Implant therapy eg after loaded Iridium wires, as will the concept of Brachytherapy. Radiotherapy timing & dosing schedule is very important as is the total number of treatments required. The important role of surgery in removing Keloid tumours where appropriate in combination with radiation. Knowledge of the acute and possible late effects of radiation need to be understood.
Publications:
- Treatment of Keloids by Surgical Excision and immediate Postoperative Single Fraction Radiotherapy. Ragoowansi, Cornes, Moss, Glees. Plastic and Reconstruct Surgery 2003; 111; 1853-1859
- Retrospective Analysis of Treatment of Unresectable Keloids with Primary Radiation Over 25 Years. Malaker, Vijayraghavan, Hodson, Yafi. Clin Oncol (2004) 16: 290-298
- The Future of Treatment for Benign Disease with Superficial Radiotherapy in The UK in the 21st Century? Glees & Weatherburn. Presentation 25th April 2017 Thinktank, Birmingham, Uk. Organised by IPEM’s Radiotherapy Special Interest Group.
- 2nd International Keloid Symposium. Rome, Italy, 2018. Four Decades of Experience with Radiation Therapy in Treating Keloid Lesions at The Royal Marsden Hospital, London, St George’s University Hospital, London and Cancer Centre London Parkside. Current Procedures and Potential for Future Developments. June 7-8, 2018. Glees, Kothandan, Furness, Fleming, Weatherburn.
- Radiotherapy dose Fractionation 2nd Edn. Royal College of Radiologists 2016.
- Radiotherapy for Non-Malignant Disorders. Textbook. Springer, 2008 Seegenschmiedt et al
- A Review of the Use of Radiotherapy in The UK for The Treatment of Benign Clinical Conditions and Benign Tumours. Royal College of Radiologists 2015
- Early Dupuytren’s: Superficial Radiotherapy offers long term Resolution without Hand Surgery. Glees, Kothandan, Weatherburn, Mackay. ESTRO 35 (29) 1465-EP 2016.
Clinical Science
Hidden Epidermal Cyst Formation Below The Umbilical Circular Keloid
Young-Jun Choi M.D.1
Keywords: Epidermal cyst, Keloid, Laparoscopy, Umbilicus.
As many surgical operations have been replaced by laparoscopic surgery, the number of umbilical keloid patients is gradually increasing. Thick keloids make accurate physical examination challenging, so clinical identification of an underlying epidermal cyst can usually be difficult. In addition, the keloid itself is thick, so it is difficult to detect even secondary inflammation. For these reasons, rapid and appropriate surgical intervention can be delayed in numerous umbilical keloid patients.
I experienced three cases of hidden epidermal cyst formation below an umbilical circular keloid. In two middle-aged women with tenderness of the keloid, an inflammatory epidermoid cyst was identified by incisional biopsy. Both patients were treated by empirical antibiotics and pus drainage with sterile packing dressing. The other case was a 78-year-old man presenting with a several year history of recurrent pain and discomfort around an umbilical keloid. An ultrasonography revealed the epidermal cyst below the keloid scar. During the operation, a well-demarcated cystic mass with hair follicle invagination was noticed, which was confirmed by an epidermal cyst on histopathological examination.
Hyperbaric Oxygen Therapy Improves The Effect Of Keloid Surgery And Radiotherapy By Reducing The Recurrence Rate
Kexin Song, MD
Objective: Keloids are exuberant cutaneous scars that form due to abnormal growth of fibrous tissue following an injury. The primary aim of this study was to assess the efficacy and mechanism of hyperbaric oxygen therapy (HBOT) to reduce the keloid recurrence rate after surgical excision and radiotherapy. Methods: (1) A total of 240 patients were randomly divided into two groups. Patients in the HBOT group (O group) received HBOT after surgical excision and radiotherapy. Patients in the other group were treated with only surgical excision and radiotherapy (K group). (2) Scar tissue from recurrent patients was collected after a second operation. Hematoxylin and eosin (H&E) staining was used to observe keloid morphology. Certain inflammatory factors (interleukin-6 (IL-6), hypoxiainducible factor-1α (HIF-1α), tumor necrosis factor-α (TNF-α), nuclear factor κB (NF-κB), and vascular endothelial growth factor (VEGF)) were measured using immunohistochemical staining. Results: (1) The recurrence rate of the O group (5.97%) was significantly lower than that of the K group (14.15%), P<0.05. Moreover, patients in the O group reported greater satisfaction than those in the K group (P<0.05). (2) Compared with the recurrent scar tissue of the K group, the expression levels of the inflammatory factors were lower in the recurrent scar tissue of the O group. Conclusions: Adjunctive HBOT effectively reduces the keloid recurrence rate after surgical excision and radiotherapy by improving the oxygen level of the tissue and alleviating the inflammatory process.
Combination Of Botox And Fat Transplantation As A New Approach In Treating Keloids, Report Of 30 Consecutive Patients
Minliang Chen, MD
Keloids are the results of abnormal wound healing. There are usually surgical and non-surgical treatment options used in clinical setting. But there is still not a satisfying treatment approach against keloid. Future developments in molecular biology and cytogenetics will hopefully pave the way for biological treatments that may not be too far on the horizon.
Objective: To explore the clinical effect towards combination of Botox and fat transplantation in keloid treatment.
Methods: thirty patients received this combined treating approach. In the 3rd postoperative followup time, thickness, color and texture was measured, pathological examination was also performed to evaluate the new approach.
Results: all keloids were ameliorated with less syndromes. After 6 months, no recurrence was found.
Conclusion: combination of Botox and fat transplantation is a new approach in treating keloid, which has good clinical effect. The new method is easy and with less complication.
Biological Approach To The Treatment Of Keloids : Recycled Concept And Technology
Kamalendu Malaker1,2,3, Mustafa Zaidi2, Rida Franka2, Twafic Alyaffi3
INTRODUCTION
Clean, surgical excision followed by postoperative radiotherapy is the most predictable successful treatment of keloids. Primary surgical excision, radiotherapy, intralesional instillation of multitudes of agents, pressure and cryo-therapy all have poor results. We set out to identify any biological pathway that may be enhanced for benefit of treatment of keloids. Since the level of oxygenation is directly related to radiotherapy response, we attempted to study the differential blood supply of keloids and surrounding normal tissue.
MATERIALS AND METHODS
Study of Histopathology Sections: Differential Vasculature between Keloids and Normal Skin
Observation
- Vascular density is much less in keloids compared to its normal adjacent skin, studied in H&E sections of both keloids and normal skin.
- Separation between blood vessels in keloids are much bigger compared to its normal skin counterpart.
- Thickness of keloidal arterial wall is 2 to 3 times more than those in normal skin indicating restricted diffusion of O2. That is, keloidal tissue are less oxygenated compared to normal skin.
Experimental Studies
- Thermography: To map and quantitate comparative vascularity. (Image-able but Unquantifiable, hence, abandoned)
- Surface Temperature Measurement as Indicator of Blood Supply and Oxygenation. Using strip thermometry, average keloid surface temperature is 95.0 ºF, whereas average skin temperature is 95.8 ºF. After two minutes of manipulation, the average keloid temperature remains the same at 95.0 ºF, while the average skin temperature changes to 97 ºF. A two degree (2 ºF) rise after manipulation in normal skin indicates 1.5 to 2 degrees differential between higher blood supply in skin than the surface of keloids. This indicate poor rheological response in keloids, which translates into hypoxic steady state of keloid.
- Measurement of Differential Fluid Content in Keloids and Normal Skin: The experiment showed 3 to 7 times more fluid content in normal skin when compared to keloids. This indicated less blood giving rise to hypoxic conditions, and poor responses to changes demanding blood. Less fluid also indicates less diffusibility of O2 and other nutrients.
- Lack of fluid (water) content indicates lack of free radical formation (Oxide Anions – O2-, Peroxide Anions – O-, Superoxide Anions – O2-) ” reduction of radio-sensitivity (chemo-sensitivity). Inference: Steady state of keloids is hypoxic and hypo-hydric, and is unresponsive to stimuli. Recommendation: Use hypoxic cell sensitizers in combination cytotoxic chemotherapy to stop keloid regrowth after surgical excision. Early results will be presented.
The Bodily Characteristics Of Keloid Patients
Jinglong Cai, MD
Abstract: Different part, degree and time of skin injury usually cause different ending. Some of them are physiological scars, some of them are hypertrophic scars and others are keloid. In this case, the author demonstrated a new theory of the body characteristics of keloid patients. To avoid skin injury is the key in getting rid of keloid which also needs early treatment. According to the characteristics of keloid, the author also offered a new type of keloid classification and treatment choices.
Surgery
Update: Multi-Modality Treatment Protocol for Ear Keloids
Lamont R Jones, MD, MBA
Learning objectives:
- At the conclusion of this activity, the participant should be able to: Discuss the pathophysiology and clinical characteristics of ear keloids.
- At the conclusion of this activity, the participant should be able to: Discuss the up to date literature on multi-modality treatment of ear keloids.
Objective: To describe the authors multimodality treatment protocol for ear keloids.
Skin Expansion In Scar/Keloid Repairing
Shuzhong Guo, MD
Chinese plastic surgeons often see scar patients after injury, especially keloid patients. The traditional approaches for Chinese patients usually not satisfying, cause the color change after surgery. We used the skin expansion technique for Chinese scar or keloid patients after a series of implantation, injection and transferring expanded skin flap, which has achieved good clinical effect. In this article, the author will introduce the improvement of skin expansion technique.
The Utility Of Skin Flaps In The Management Of Large Keloid Lesions
Xin Xing, MD
Scars developing on body surfaces not only restrict body movement, but are also problematic from a cosmetic standpoint. skin flaps are one of the fundamental techniques in scar revision. In this paper, I will introduce my experience in scar revision by various skin flaps, including Z-plasty, W-plasty, V-Y plasty, A-T plasty, modified Limberg flap, nasolabial flap, paranasal flap, subcutaneous pedicle flap, island flap, expended flap and free flap, et cetera.
The Suture Techniques : The Details And Improvements In Plastic Surgery
Junli Shi, MD
Objective: To obtain and recommend a new wound suture technique which can effectively prevent the formation of hypertrophic scar and promote wound healing.
Methods: Trapezoidal wound excision technique combined with improved buried vertical mattress suture technique was used to suture common wounds and tension wounds. After a long-term multi-center comparative study, the design of the same patient was compared with conventional excision and suture techniques.
Result: The combination of trapezoidal resection and improved buried vertical mattress suture technique can make the incision margin get exact effect of reducing tension. The incision margin has good combination, good valgus and minimal intradermal foreign body retention. Compared with conventional resection and suture techniques, our improved technique has achieved better results in the same patient.
Conclusion: Trapezoidal incision combined with our improved vertical mattress submerged suture technique can prevent the formation of hypertrophic scar, and it is the most important surgical procedure to prevent the formation of scar.
Abstract Presentations
Preliminary Investigation On The Distribution Of Phlegm-Dampness/ Dampness-Heat Tongue And Tcm Constitution In Keloid Patients
Haiyang Liu, MD
Abstract Objective: To investigate distributional rate difference between keloid and normal scar patients in order to explore the common constitution type of Traditional Chinese Medicine (TCM) in keloid patients.
Methods: Keloid and normal scar patients were investigated for different distribution rate of phlegmdampness( PD)/dampness-heat(DH) tongue and TCM constitution (TCMC) according to the diagnostic image of TCM tongue and “The criteria for classification of TCMC” as well as keloid conditions, and the difference was statistically analyzed with Chi-square test.
Results: The distribution rate of PD/DH tongue and TCMC was significantly higher in keloid than in normal scar patients. Additionally, the distribution rate was also significantly higher in the patients with spread multiple keloids than those with localized single keloid. Moreover, PD/DH tongue appeared more frequently in keloid patients who also possessed PD/DH TCMC. For all investigated patients who were both positive for PD/DH tongue and TCMC, 81.5% were keloid patients, whereas only 18.5% were normal scar patients.
Conclusion: Keloid patients are more prone to PD/DH TCMC, a type of chronic inflammatory constitution of modern medicine, which may contribute to keloid origin and development.
The In Vitro And Ex Vivo Anti- Keloid Activity Of Sorafenib By Antagonizing TGF-β/Smad And MAPK/ERK Signaling Pathways
Wenbo Wang, PhD
Abstract: Keloid disease is characterized by hyperproliferation of responsive fibroblasts with vigorously continuous synthesis of extracellular matrix (ECM) components. Although the process by which keloids develop is poorly understood, most theories of the etiology are referred to fibroblast dysfunction. A central event in dermal repair is the release of growth factors in response to skin injury, which leads to the dysregulation of several crucial pathways that initiate the activation of keloid fibroblasts (KFs) and promote ECM accumulation. Hence, strategies aimed at reducing the production of these cytokines and/ or disrupting their intracellular signal transduction have potential clinical significance for curing keloid. As the first oral multi-kinase inhibitor, sorafenib blocks a number of intracellular signaling pathways which are also pivotal for keloid pathogenesis. Therefore, evaluation of the effects of sorafenib on keloid disease seems timely and pertinent. In this study, we reported the identification of sorafenib that antagonized TGF-β/Smad and MAPK/ERK signaling pathways in primary KFs. Impressively, treatment with sorafenib inhibited KF cell proliferation, migration and invasion, and simultaneously reduced collagen production in KFs. Furthermore, we present ex vivo evidence that sorafenib induced the arrest of KF migration, the inhibition of angiogenesis and the reduction of collagen accumulation. These preclinical observations suggest that sorafenib deserves systematic exploration as a candidate agent for the future treatment of keloids.
Key words: sorafenib, keloids, keloid fibroblast, TGF-β/Smad signaling, MAPK/ERK signaling.
Evidence About Halofuginone Interest For Keloid Treatment
Marty P.1,2,3, Chatelain B.2, Isidoro Ciro4, Meyer C.2, And Rolin G.1,3*
* Contact information
Dr. Gwenaël ROLIN, PhD
Hospital Research Engineer
INSERM CIC-1431, University Hospital of Besançon,
Clinical Investigation Center
2 place St Jacques – 25000 Besançon
grolin@chu-besancon.fr
Office: +33 (0)3 81 21 91 64 / Mobile: +33(0)6 84 25 77 92
Keloids scars are fibrotic tumors resulting from an abnormal proliferation of cutaneous tissue beyond the original wound margins. Considered as chronic inflammatory diseases, keloids do not regress over time, exhibit high recurrence after surgery and do not currently benefit from effective therapy [1]. On one hand, fibroblasts are one the key cells involved in keloid pathogenesis. Keloid fibroblasts exhibit a fibrotic phenotype compared to their healthy counterpart and strongly differ according their location in the keloid center or periphery [2]. On the other hand, halofuginone (HF) has been described as a promising anti-fibrotic and anti-inflammatory molecule which inhibits Smad3 phosphorylation downstream of the TGF-β signaling pathway and prevents of Th17 cell differentiation [3]. However, the potential of HF on keloids [4] has not been investigated yet despite evidences about HF’ role as TGF reversing agent of the fibrogenesis progression. We propose here to review the literature in order to highlight published data about HF antifibrotic effect and to give up to date evidence proving that halofuginone is an interesting candidate for keloid prevention and treatment.
- Lee HJ and Jang YJ. Recent Understandings of Biology, Prophylaxis and Treatment Strategies for Hypertrophic Scars and Keloids. Int J Mol Sci. 2018. 19, 711.
- Jumper N, Hodgkinson T, Paus R and Bayat A. Site-specific gene expression profiling as a novel strategy for unravelling keloid disease pathobiology. PLoS One. 2017. 12:e0172955.
- Luo Y, Xie X, Luo D, Wang Y and Gao Y. The role of halofuginone in fibrosis: more to be explored? J Leukoc Biol. 2017. 102:1333-1345.
- Lista S and Emanuele E. Potential therapeutical effects of topical halofuginone hydrobromide in keloid management. Med Hypotheses. 2007. 69:707.
The Anti-Keloid Activity Of Nintedanib By Antagonizing TGF-β/Smad and MAPK Signaling Pathways Via Lipid Raft/Caveolae
Boya Zhou, MD PhD
Objective: To investigate the effect of nintedanib on keloid fibroblasts.
Methods: Keloids fibroblasts (KFs) were isolated and cultured with or without different concentrations of nintedanib. The effect of nintedanib on the proliferation of KFs were evaluated by CCK-8, EDU incorporation assay and cell cycle analysis. The effect of nintedanib on the fibrosis gene and protein of KFs was analyzed by RT-qPCR and Western blotting. Meanwhile, this study explored whether nintedanib antagonized signaling pathways related to VEGF-Rs, FGF-Rs, PDGF-Rs such as TGF-β/Smad and MAPK pathway via lipid raft/caveolae. The scratch assay and cell invasion assay were employed to show the effect of nintedanib on the invasion of KFs. In addition, the effect of nintedanib on the collagen deposition and angiogenesis of ex vivo keloid tissue was detected by immunohistochemical staining.
Results: 1. In the experimental group, the proliferation of KFs was significantly inhibited, and the cells were arrested in the G1 phase. 2. In the experimental group, the collagen formation and deposition of KFs was attenuated. 3. In the experimental group, the migration and invasion of KFs were inhibited. 4. In the ex vivo explant culture of keloid tissue, nintedanib can inhibit the deposition of collagen and the formation of blood vessels. 5. The inhibitory effect of nintedanib on KFs is mainly through the degradation of receptors via lipid rafts/caveolae, thus blocking the TGF-β/Smad signaling pathway and MAPK pathway. Conclusion: Nintedanib can inhibit the proliferation, migration and invasion of KFs and reduce collagendeposition. These preclinical observations indicate that nintedanib can be considered as a candidate for future keloid treatment.
Key words: nintedanib, keloid fibroblast, TGF-β/ Smad signaling, MAPK signaling, lipid raft/caveolae.
Clinical Outcome Of 1064-Nm Picosecond Neodymium-Doped Yttrium Aluminium Garnet Laser For The Treatment Of Hypertrophic Scars
Young-Jun Choi M.D.1
Keywords: hypertrophic scars, laser treatment, neodymium-doped:yttrium aluminium garnet, picosecond.
BACKGROUND: Currently no study has evaluated the effect of the novel 1064-nm picosecond neodymium-doped:yttrium aluminium garnet laser (ps-Nd:YAG) for reducing hypertrophic scarring (HS). OBJECTIVE: The aim of this study was to verify the efficacy and safety of a 1064-nm ps-Nd:YAG in the management of HS.
MATERIALS AND METHODS: A retrospective chart review and photographic analysis were conducted on patients treated with a low-fluence 1064-nm ps- Nd:YAG for HS improvement. The Vancouver Scar Scale (VSS), 5-point Global Assessment Score (GAS), and patient satisfaction score were used to determine the effect of scar improvement.
RESULTS: A total of 24 Korean patients (9 males and 15 females; mean age of 33.25 ± 15.50 years) were retrospectively evaluated. Mean treatment settings were 1064-nm wavelength, 750 ps pulse duration, 7.94 mm spot size, 0.93 J/cm2 fluence, and 9.69 Hz frequency. The average VSS score decreased significantly (from 5.33 to 2.71) after laser treatment (p < 0.001). The average GAS (3.02 ± 0.93) showed fair cosmetic improvement, and patient satisfaction scores (6.88 ± 2.66) indicated moderate satisfaction.
CONCLUSION: The novel low-fluence 1064- nm ps-Nd:YAG could be considered as an effective and safe optional modality for the treatment of HS in Asian skin.
Special Sessions
Clinical Mimickers Of Keloids: A Diagnostic Pitfall
Chao-Kai Hsu1,2, Ting-Yu Yeh1,3, Hsin-San Yang1,Julia Yu-Yun Lee1
Background: Most keloids can be easily diagnosed based on the history and the clinical features of a raised erythematous plaque or tumor extending beyond the original border of the skin wound. However, keloids may occasionally be confused with other neoplastic or inflammatory disorders. Therefore it is important to be aware of potential clinical mimickers of keloid to avoid misdiagnosis and inappropriate treatment.
Methods: We searched our department database (July 1990-Jan 2019) for the cases with clinical diagnosis of keloid but proven to be other diagnoses pathologically. Results: A total of 25 cases were identified. There were 10 males and 15 females with age 24-69 years (mean 41.0 years). The keloid-like lesions were located on the extremities (n=8), head and neck (n=7), chest (n=5), and trunk (n=5). They were mostly asymptomatic, but 20% were itchy or painful. By pathological examination, the diagnoses were dermatofibroma (n=8), lichen simplex chronicus (n=3), metastatic carcinoma (n=3), dermatofibrosarcoma protuberans (n=2), lymphoproliferative disorders (n=2), and one each for leiomyosarcoma, basal cell carcinoma, atypical fibrous histiocytoma, angiolymphoid hyperplasia with eosinophilia, acne keloidalis, lupus erythematosus/lichen planus overlap syndrome and mycobacterial infection.
Conclusion: Our study further expands the clinicopathological spectrum of keloid mimickers, and highlights the importance of skin biopsy to avoid delay in the diagnosis and treatment.
